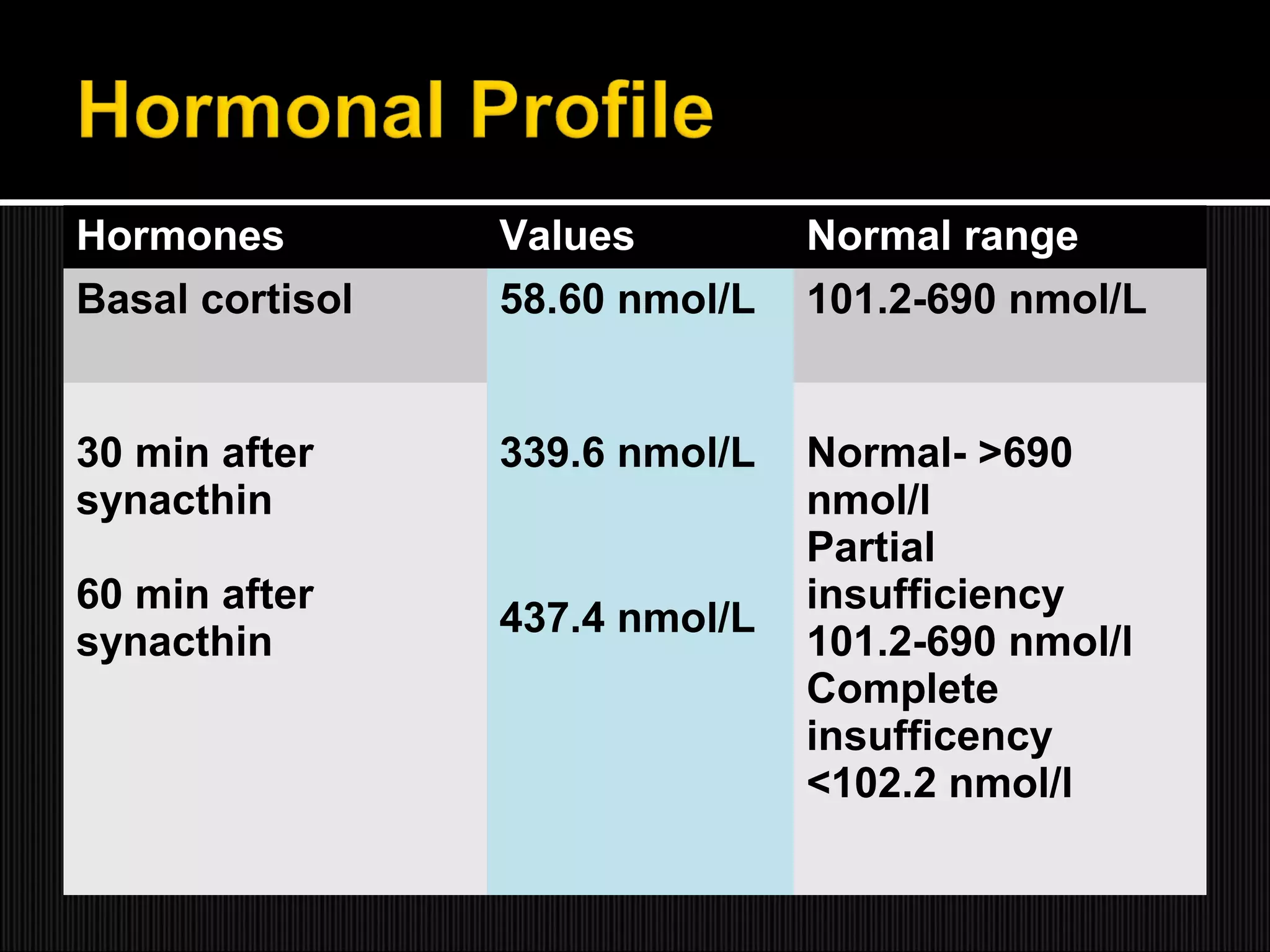
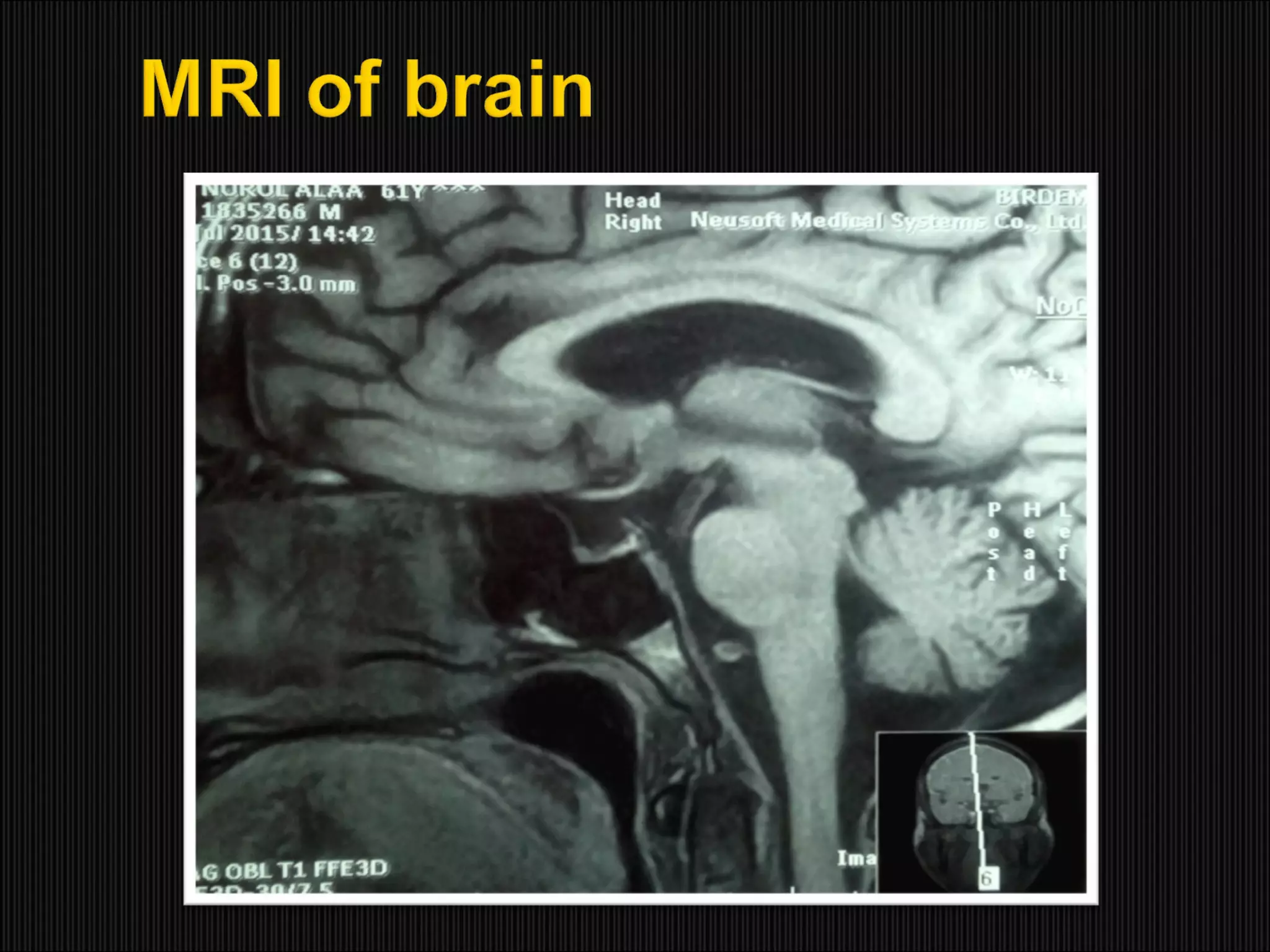
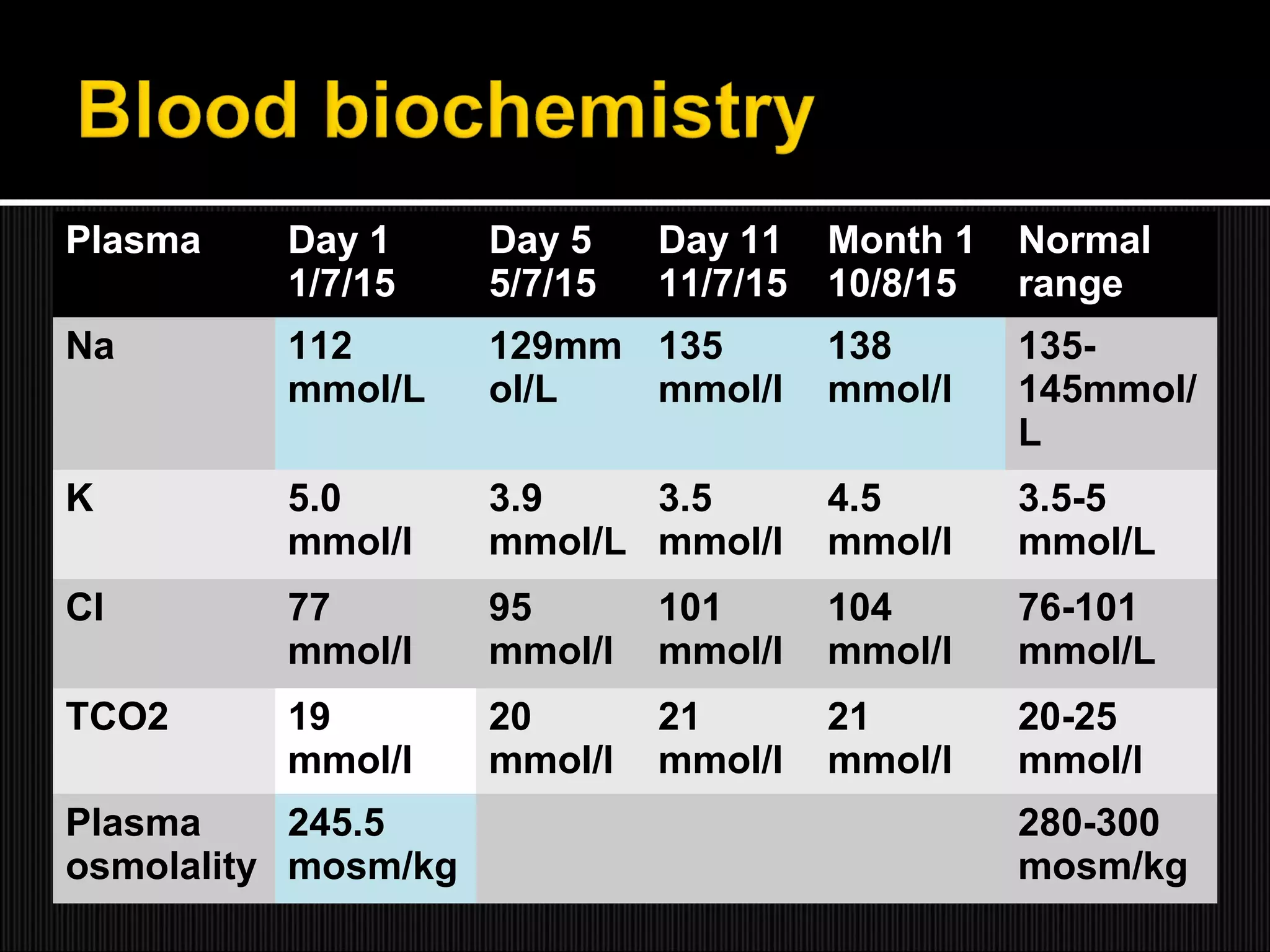
This case report describes a 61-year-old male who presented with recurrent hyponatremia. Endocrine evaluation revealed partial adrenal insufficiency and low levels of pituitary hormones. MRI showed an empty sella. Treatment with hydrocortisone supplementation normalized the sodium levels. The report discusses that hyponatremia can occur in secondary adrenal insufficiency due to empty sella syndrome, as compression of the pituitary gland can cause various endocrine abnormalities. Rapid correction of hyponatremia is possible with hydrocortisone replacement.