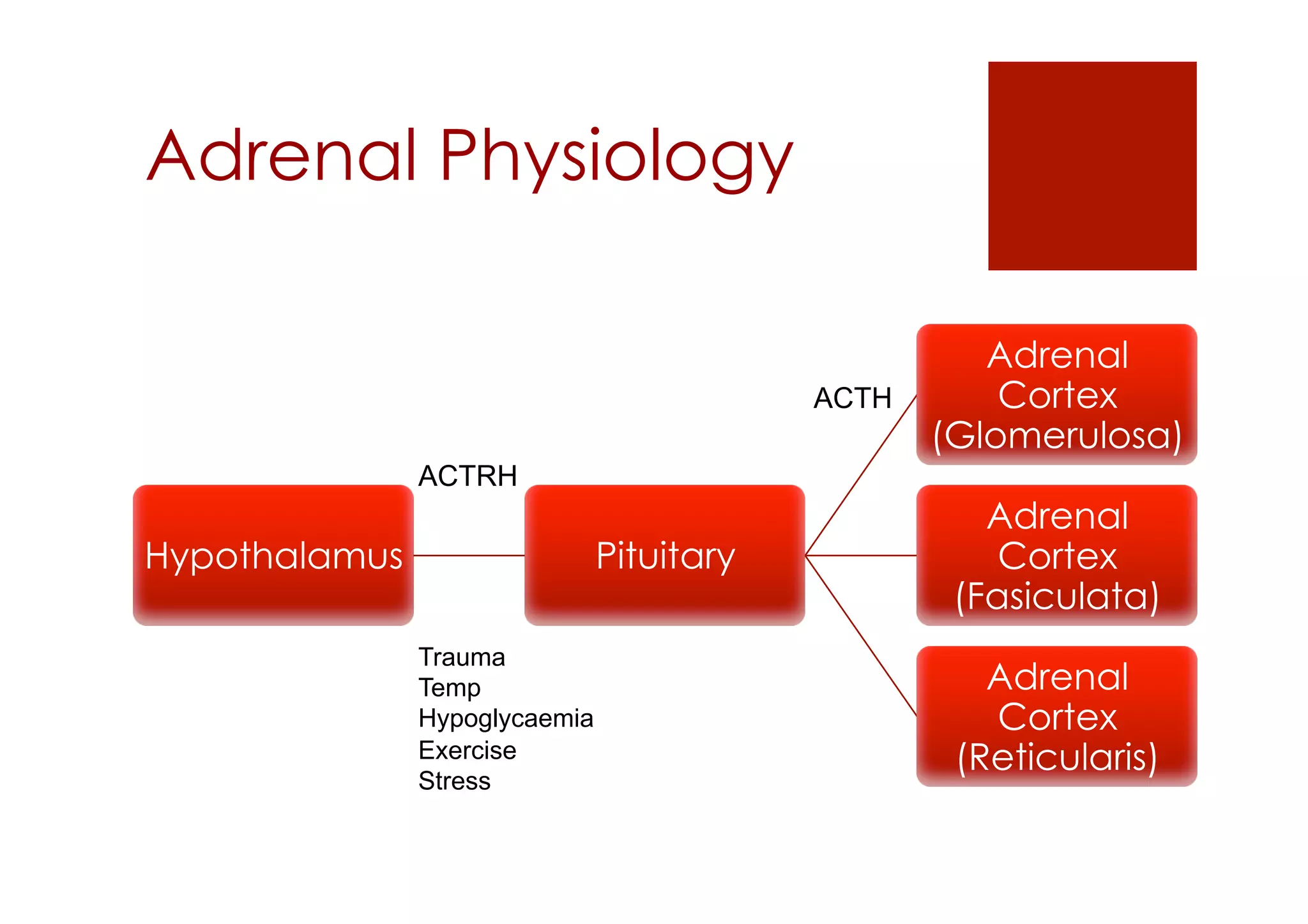
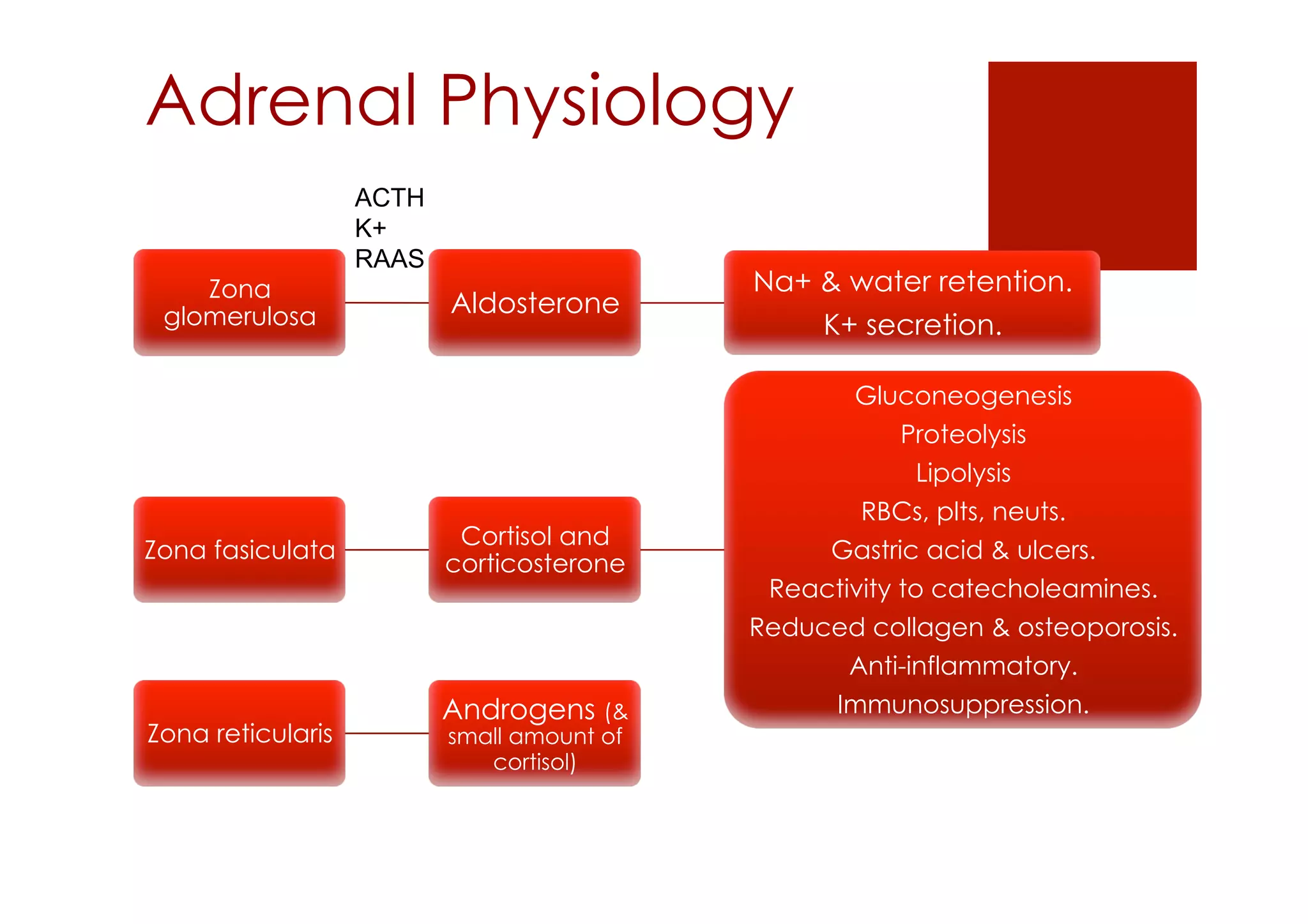
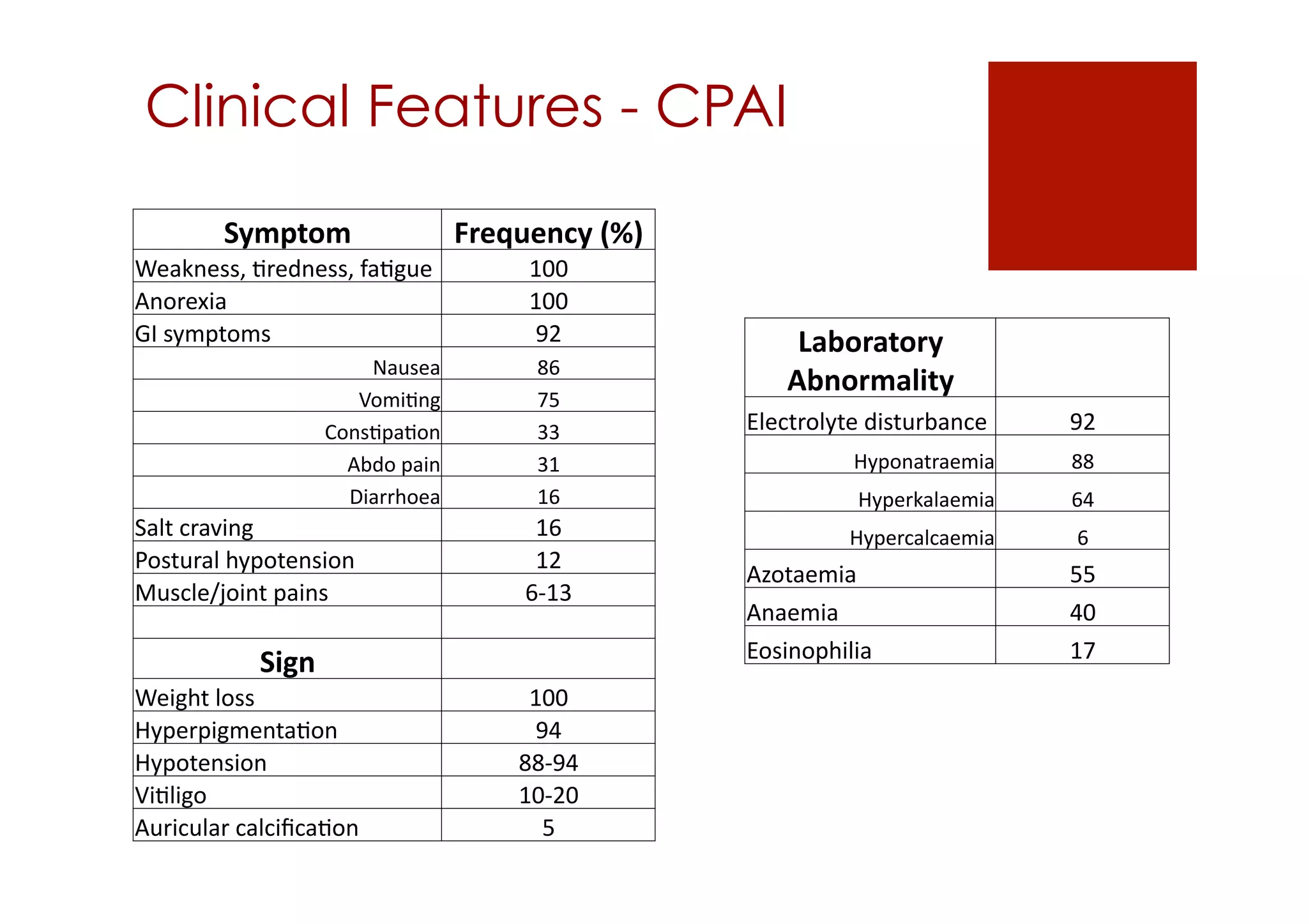
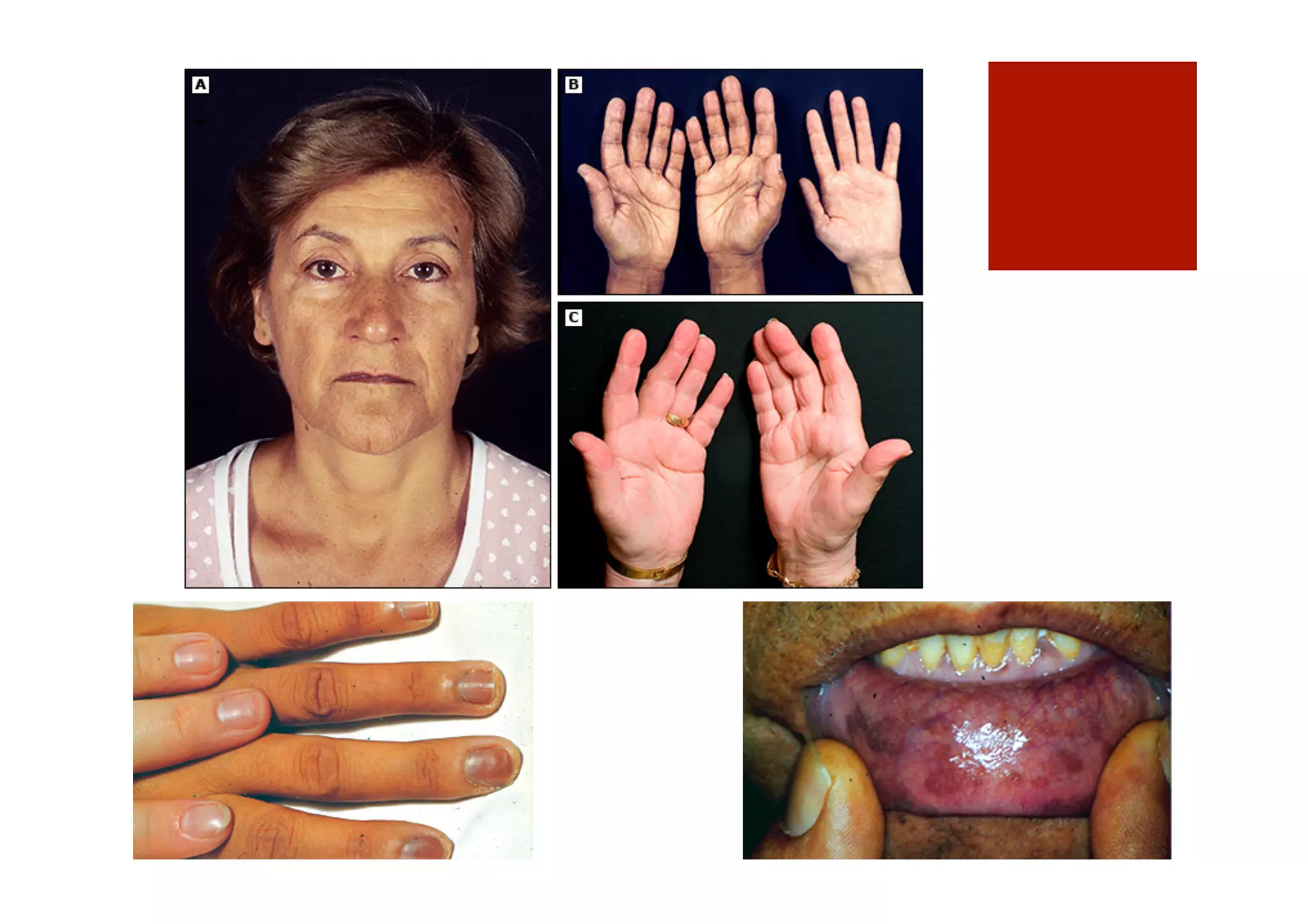
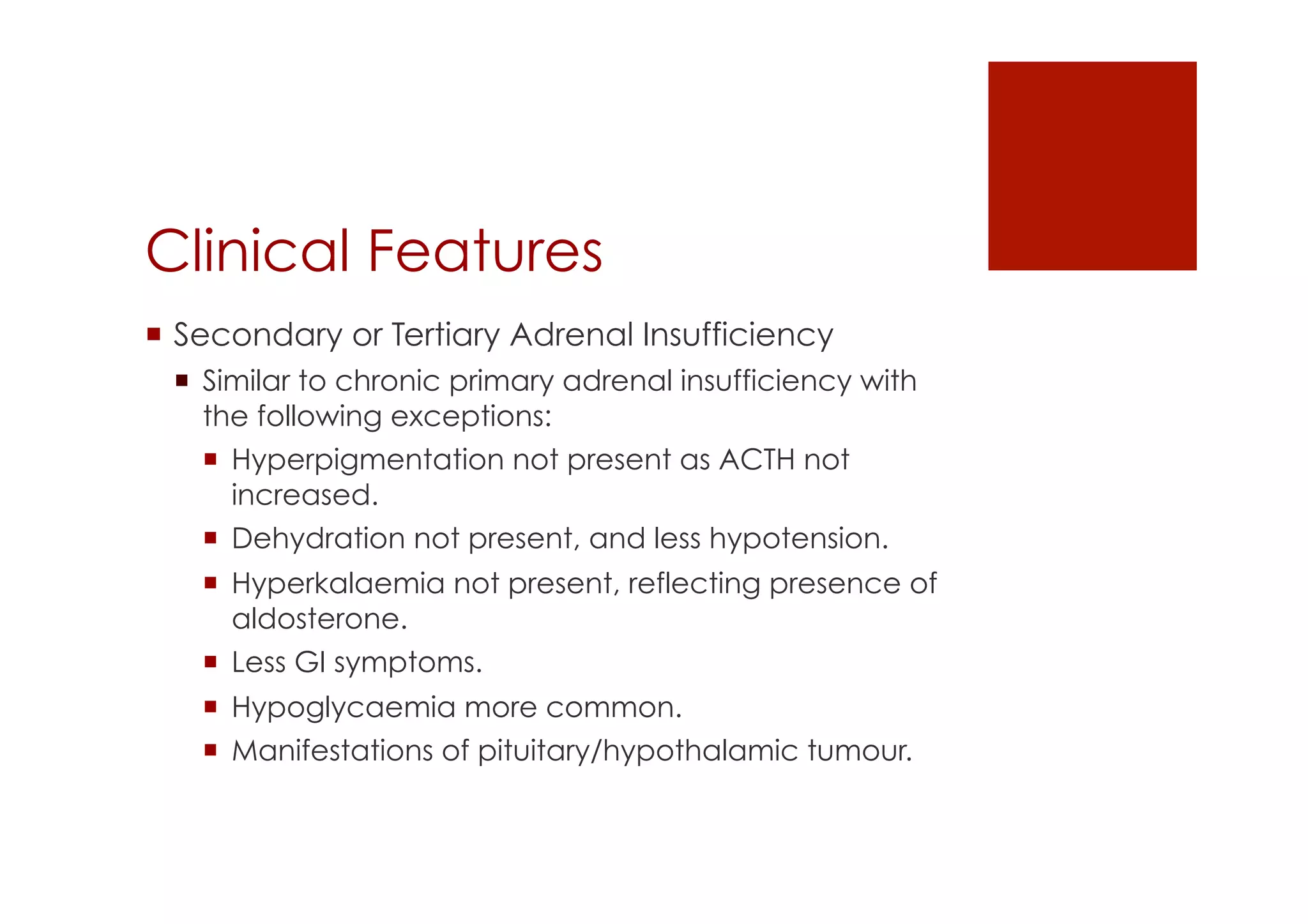
This document presents a case study of a 40-year-old man diagnosed with hypoadrenalism. He presented with nausea, vomiting, and weakness over several weeks. Initial lab results showed very low sodium and other electrolyte abnormalities. A short Synacthen test confirmed primary hypoadrenalism. He was started on hydrocortisone and fludrocortisone replacement. The document then reviews adrenal physiology, causes of hypoadrenalism including primary and secondary forms, clinical features such as adrenal crisis, and approaches to diagnosis and treatment including glucocorticoid and mineralocorticoid replacement therapy.