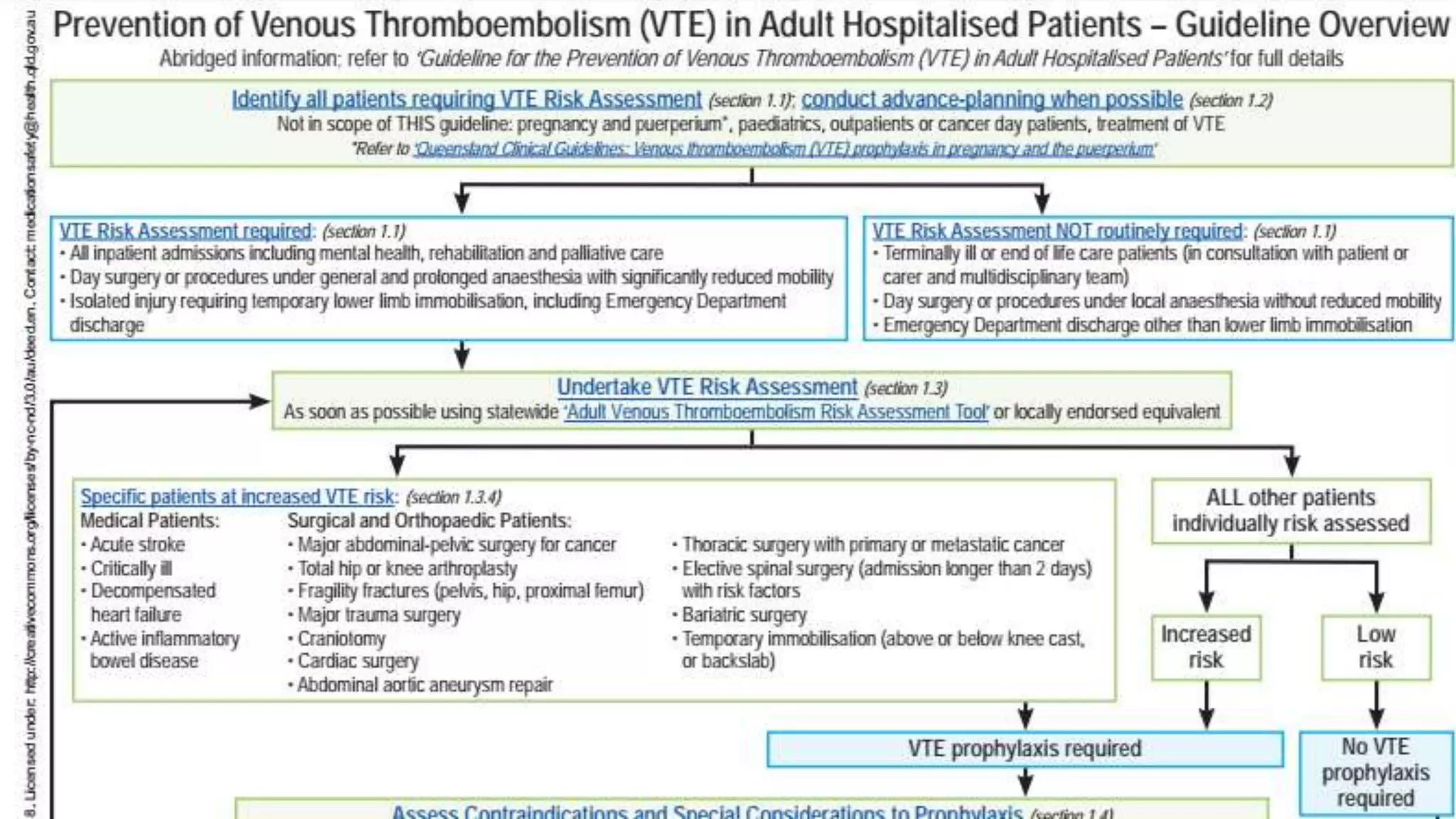
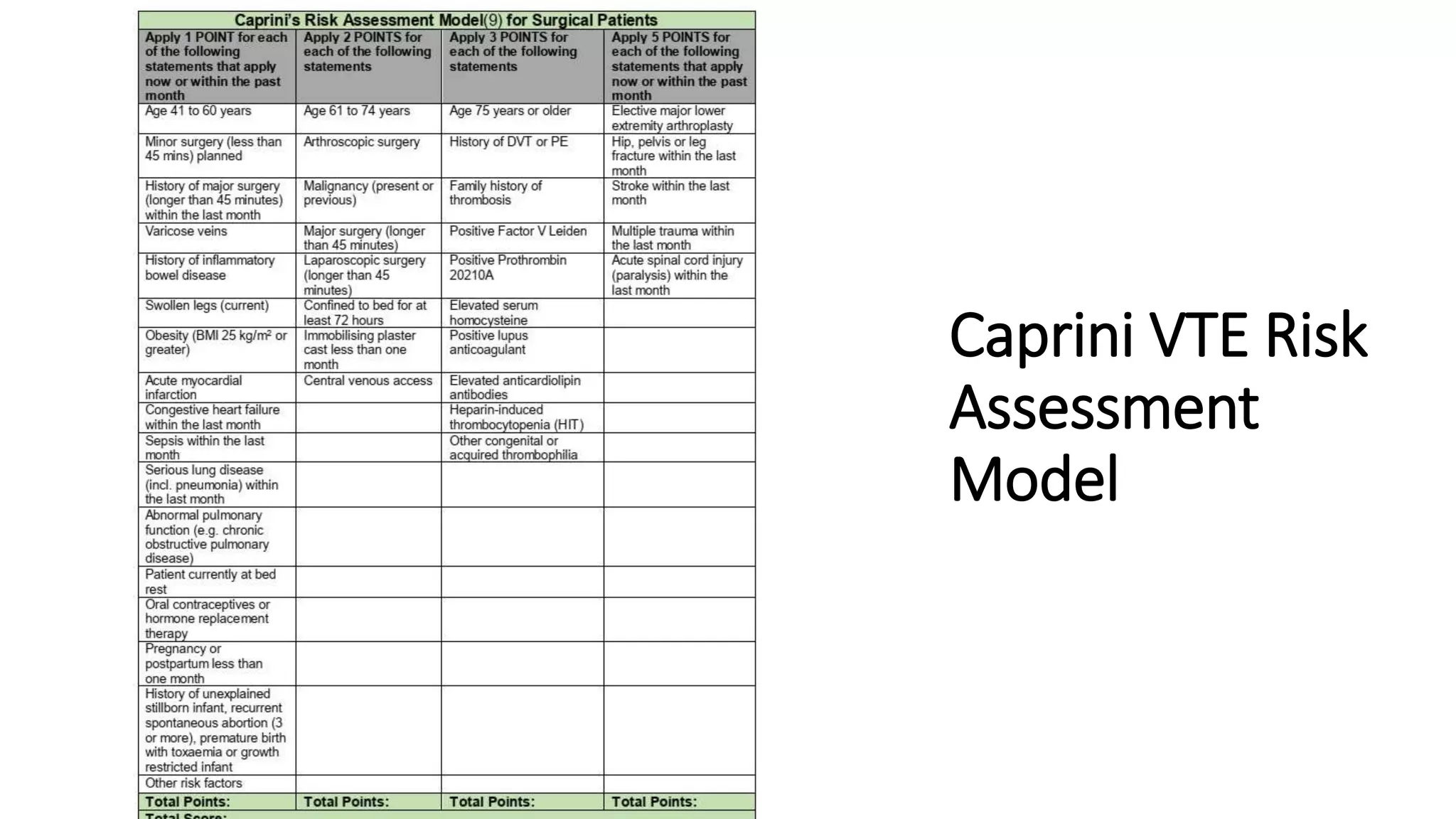
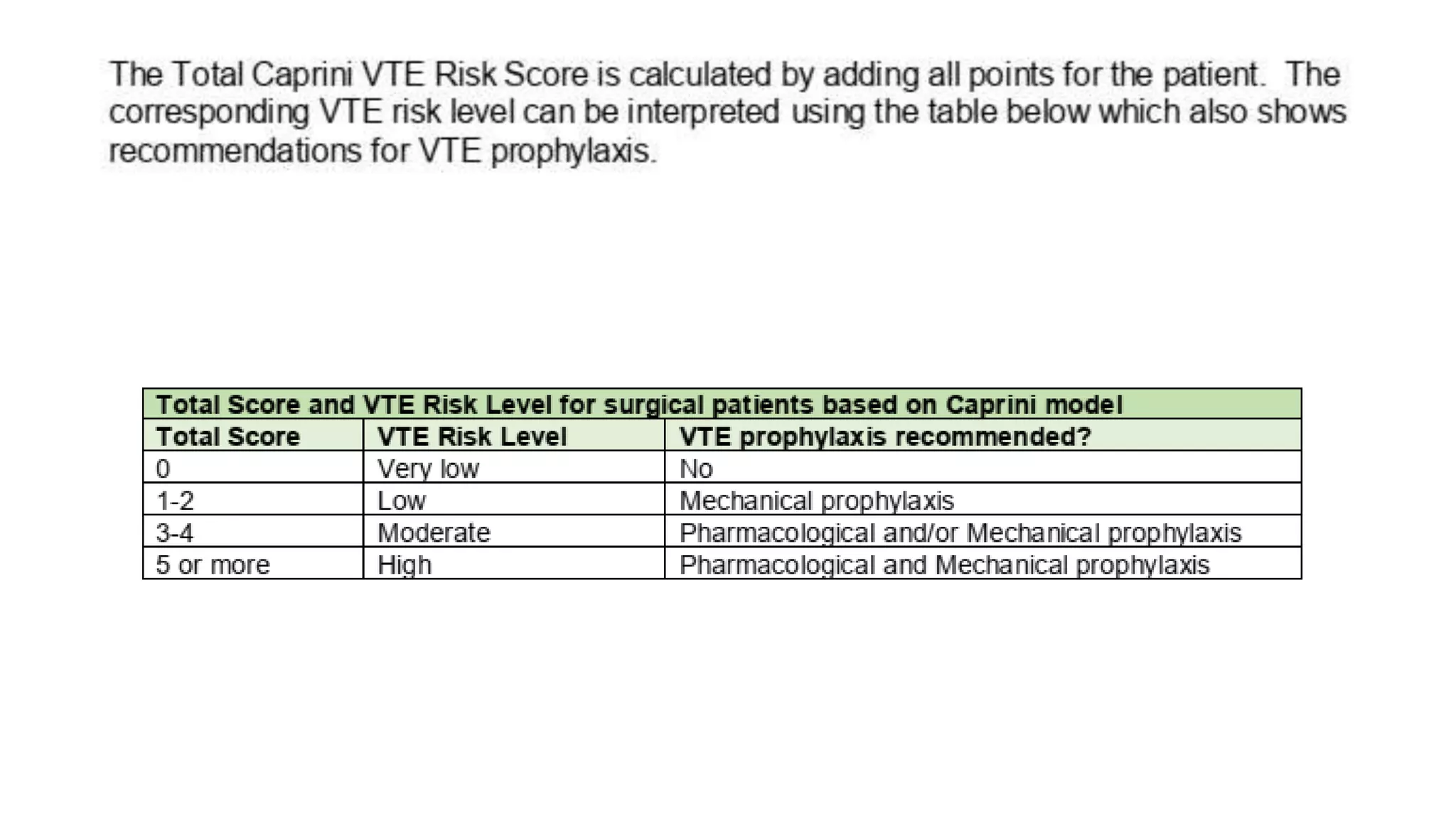
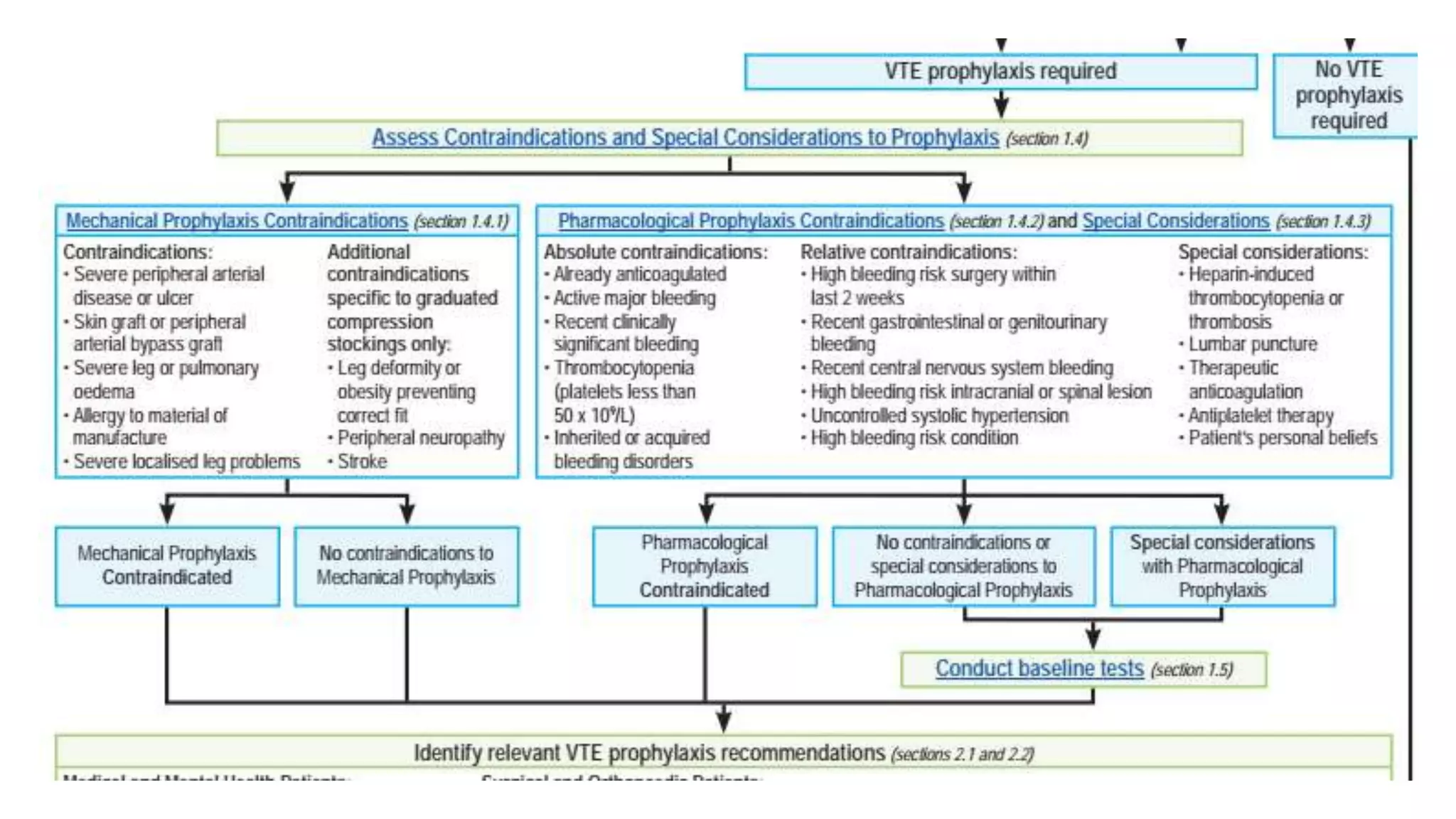
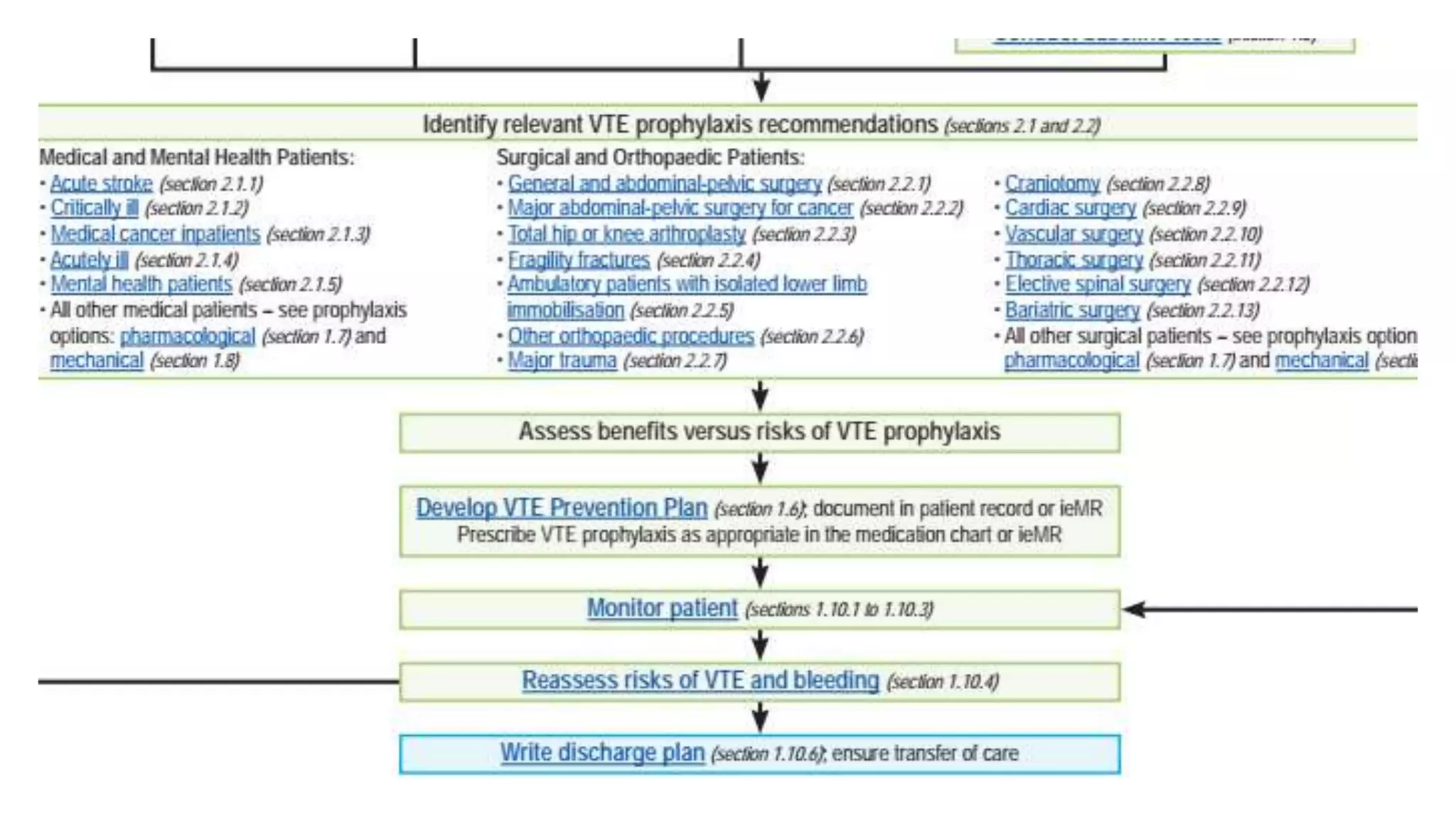
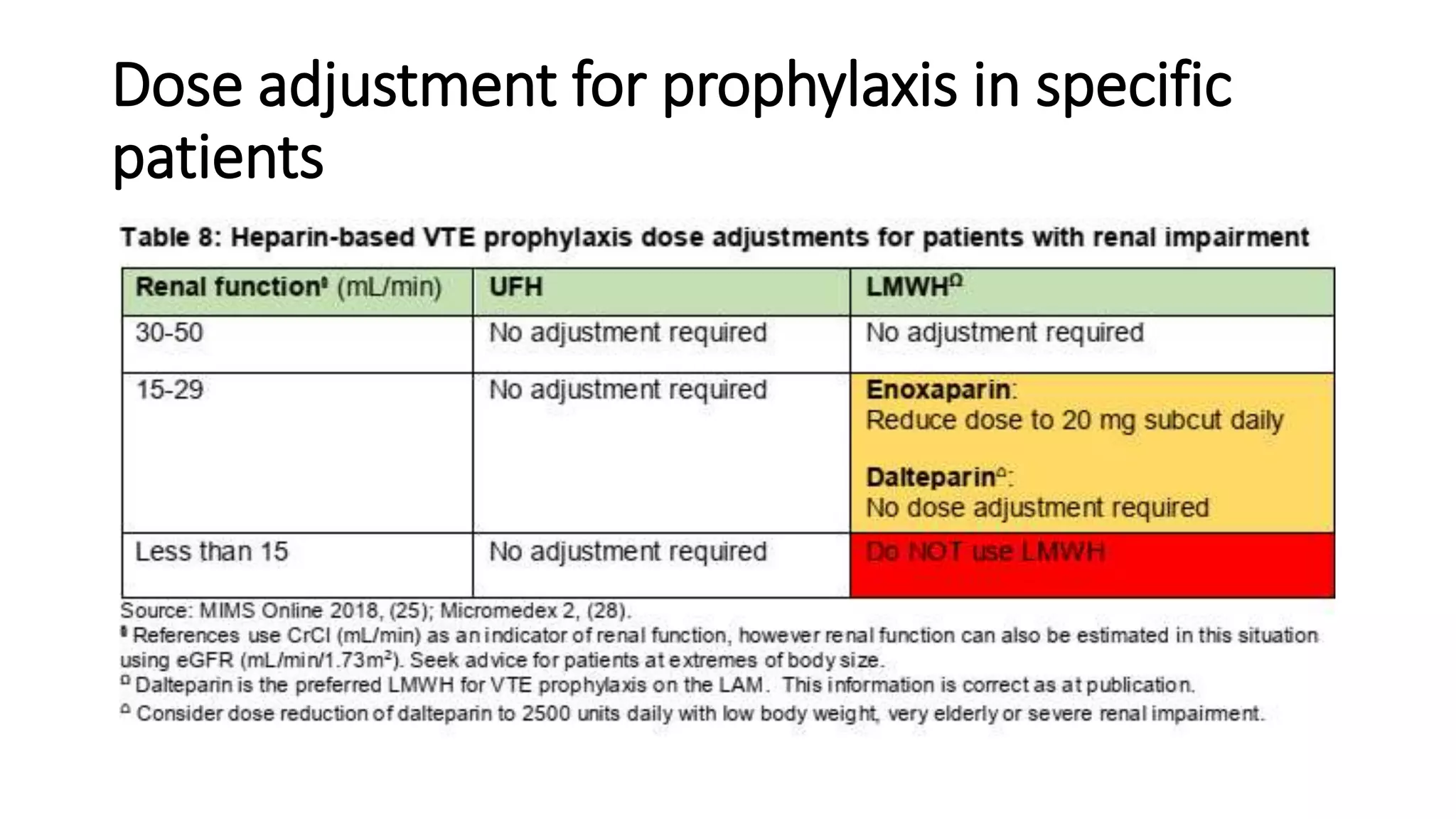
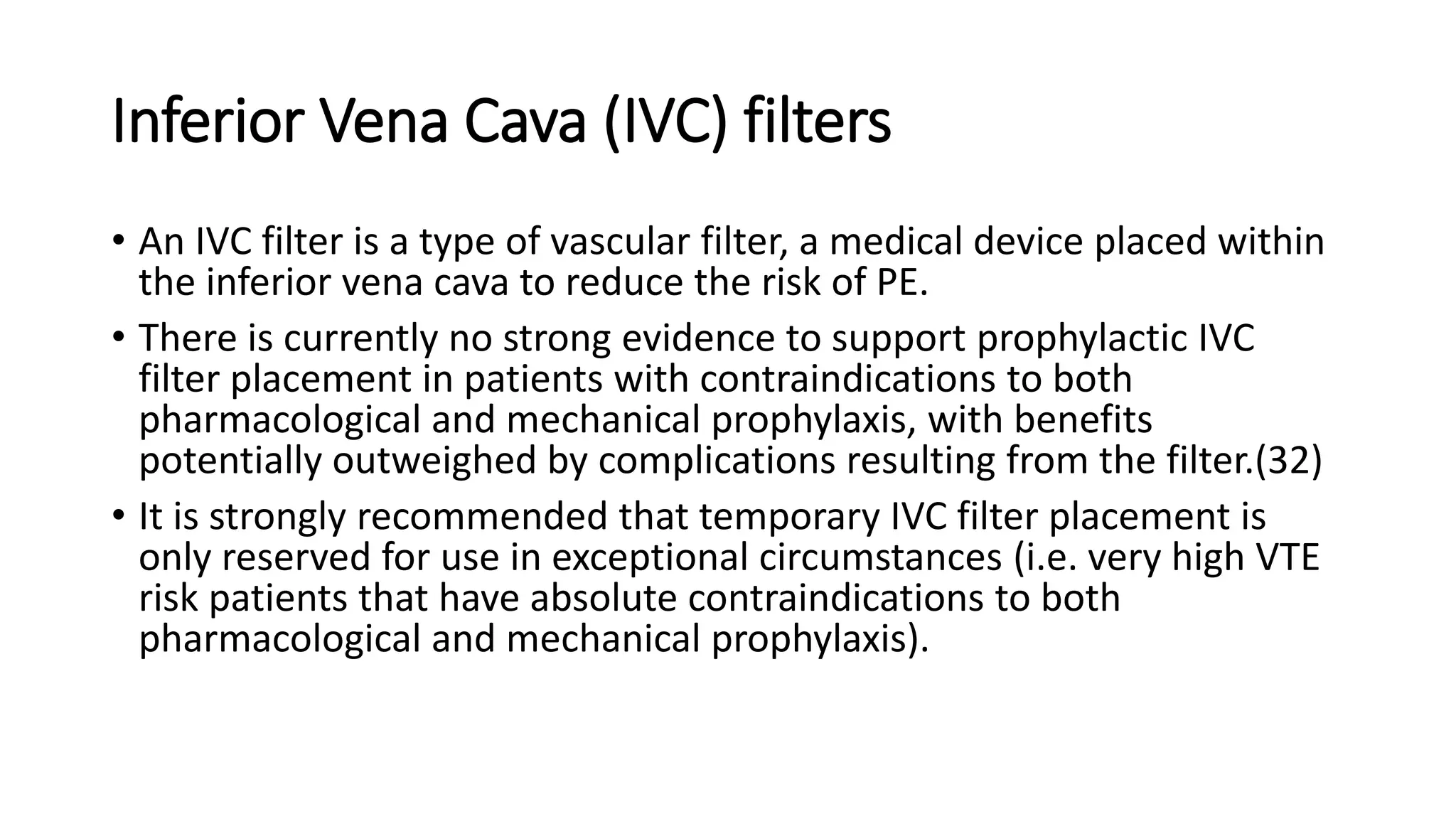
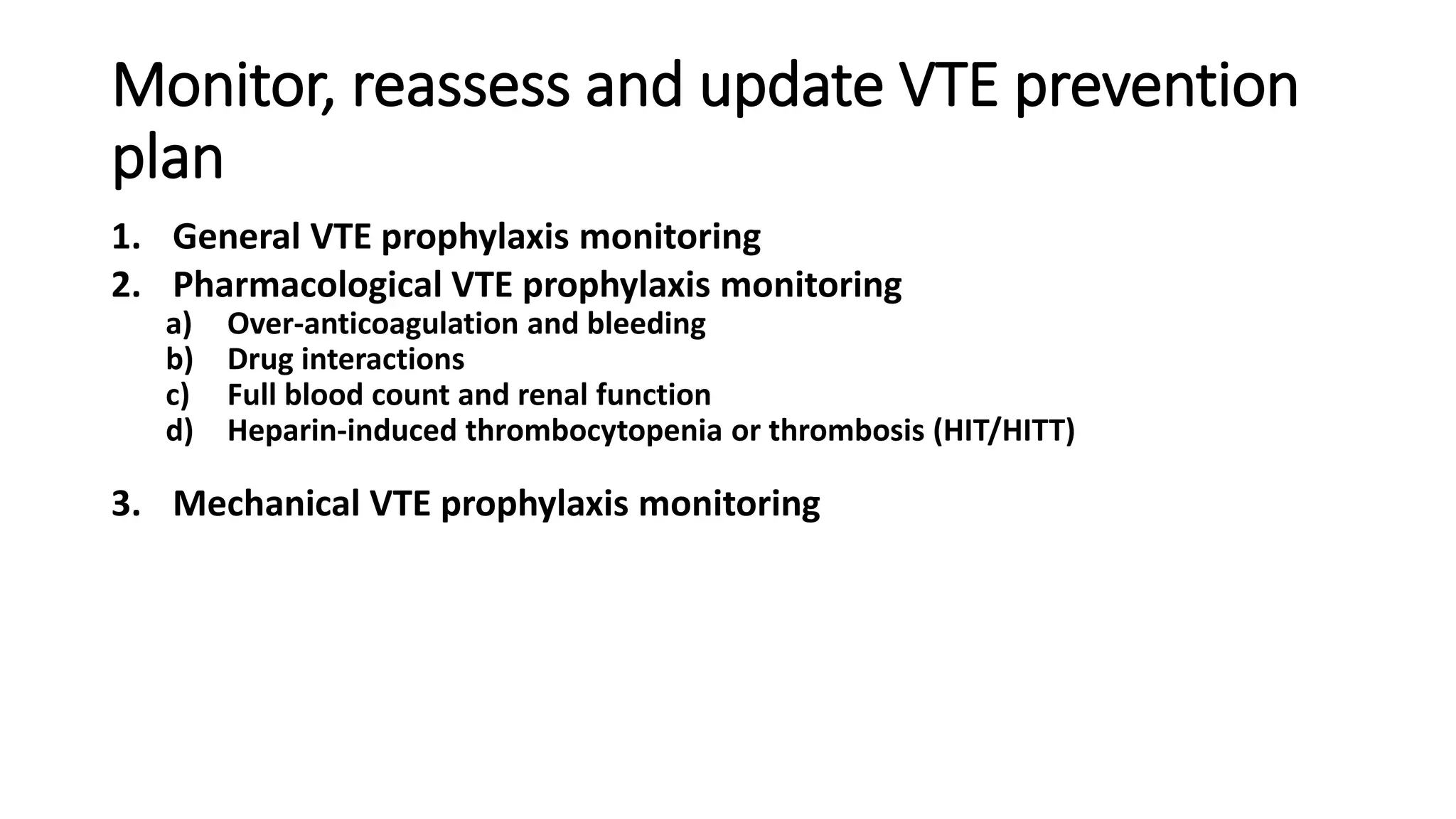
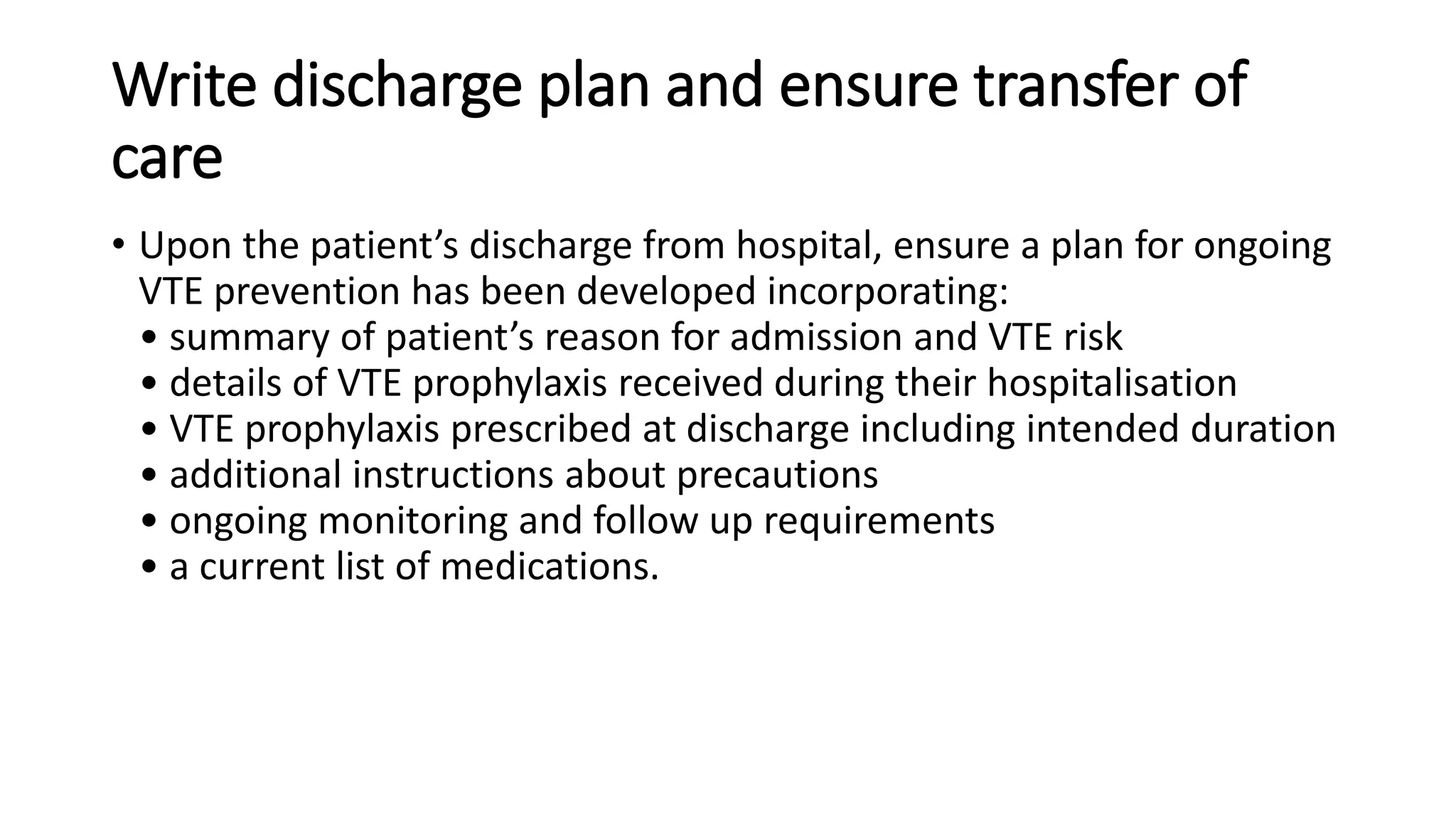
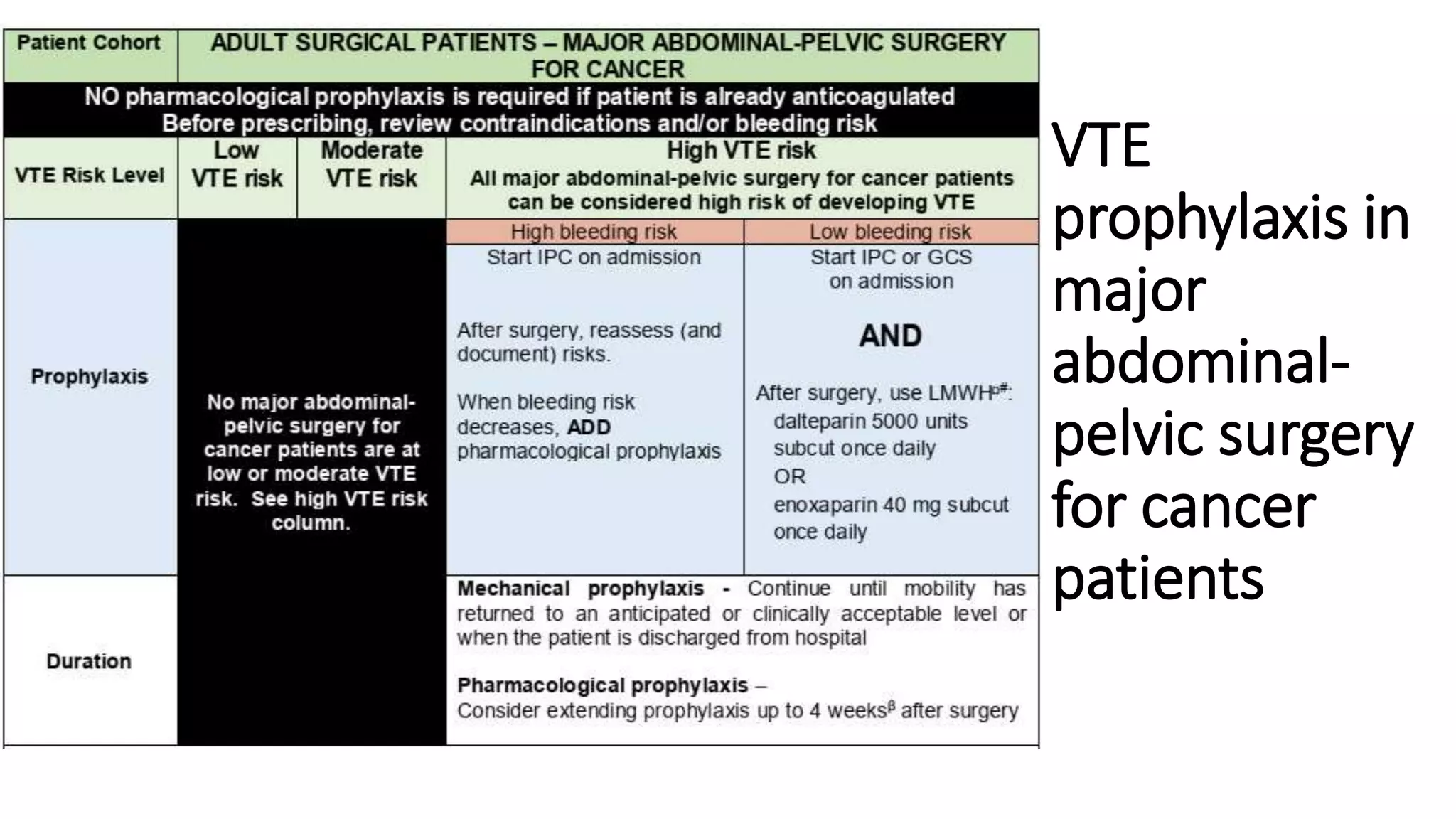
This document provides guidelines for the prevention of venous thromboembolism (VTE) in surgical patients, emphasizing the importance of VTE prophylaxis in minimizing mortality and morbidity. It outlines risk assessment models, specific patient groups at higher risk, and prevention strategies including pharmacological and mechanical prophylaxis. Additionally, it details monitoring requirements and emphasizes the need for updated discharge plans and ongoing patient engagement in VTE prevention.