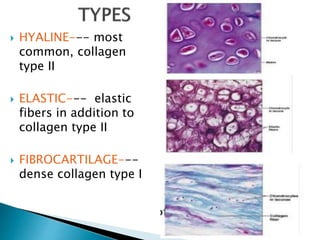
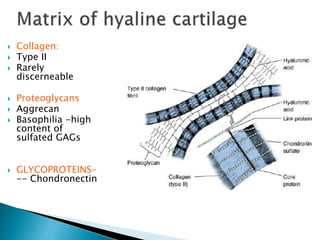
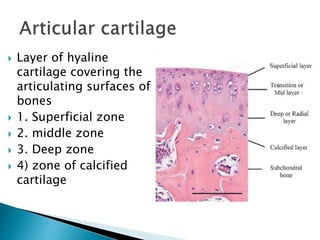
This document describes the histological features of cartilage and changes seen in degenerative diseases. Cartilage is a connective tissue that provides cushioning and gliding abilities. It consists of chondrocytes embedded in an extracellular matrix of collagen fibers and proteoglycans. The three main types of cartilage are hyaline, elastic, and fibrocartilage, which differ in their matrix composition and locations in the body. Degenerative diseases like osteoarthritis damage cartilage through loss of matrix and changes in physical properties over time.