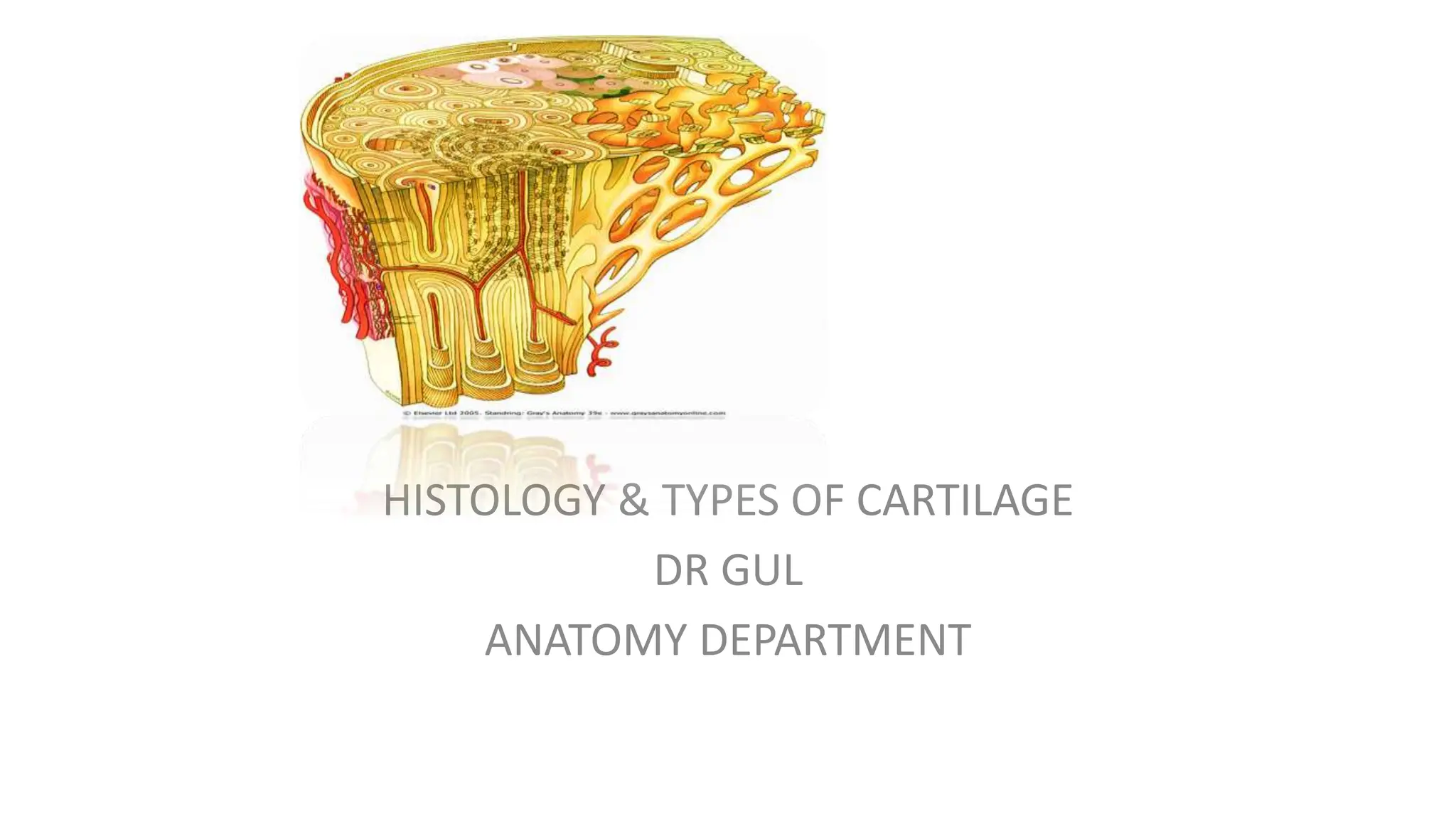
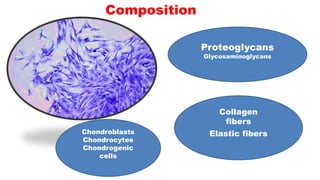
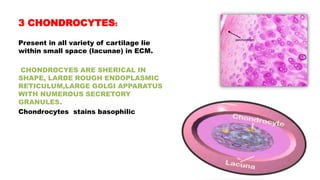
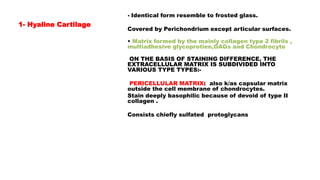
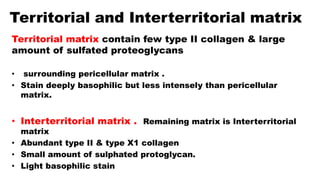
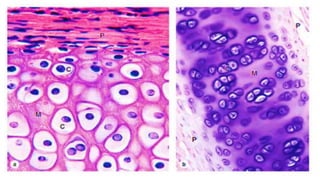
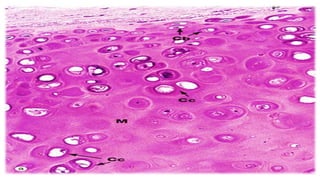
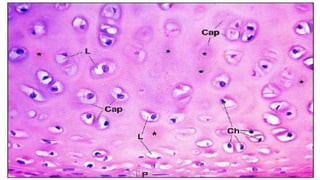
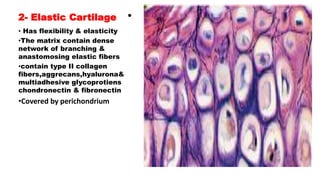
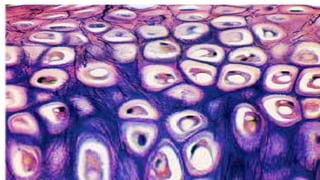
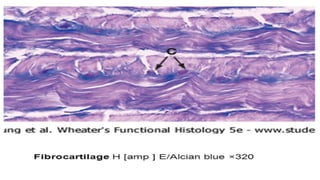
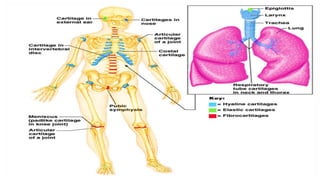
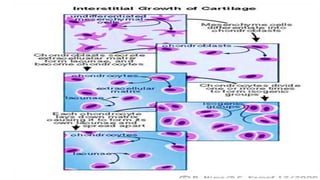
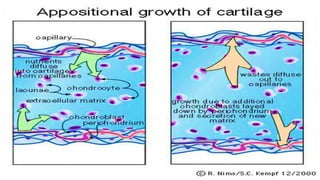
This document discusses the histology and types of cartilage. There are three main types of cartilage - hyaline, elastic, and fibrocartilage. Hyaline cartilage is found in joints and covers bone surfaces. It has chondrocytes embedded in an extracellular matrix made of collagen and proteoglycans. Elastic cartilage is found in the ear and larynx and contains elastic fibers that give it flexibility. Fibrocartilage is a mix of cartilage and dense connective tissue found in intervertebral discs and menisci where strength and flexibility are required. The document also describes cartilage composition, growth, and repair processes.