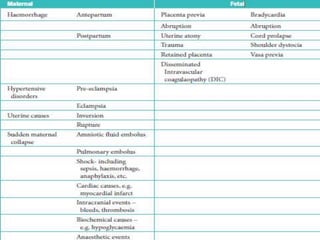
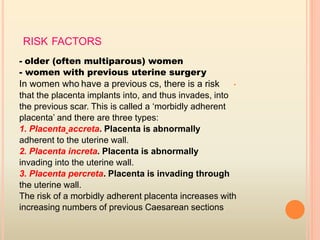
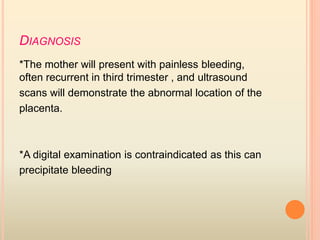
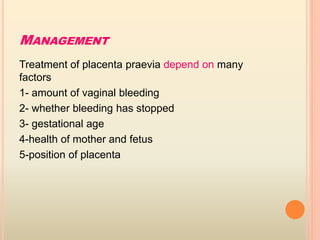
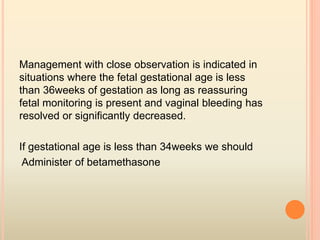
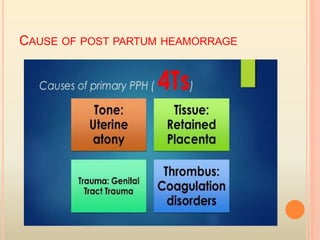
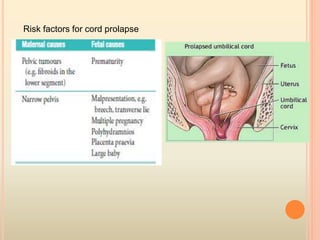
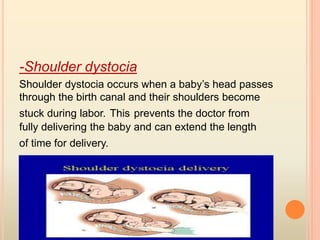
This document summarizes several obstetric emergencies, including classifications, approaches, and management strategies. Obstetric emergencies can be maternal or fetal and include hemorrhage, hypertension, uterine rupture, and cord prolapse. The structured ABC approach is recommended to initially assess and stabilize all emergency patients. Specific conditions like placenta previa require monitoring or delivery depending on bleeding and gestational age. Overall the document provides an overview of evaluating and treating common high-risk pregnancies and deliveries.