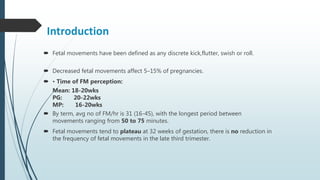
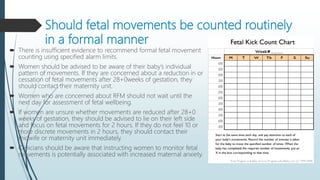
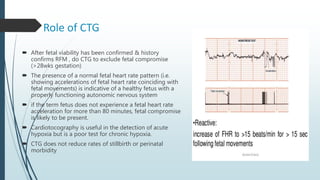
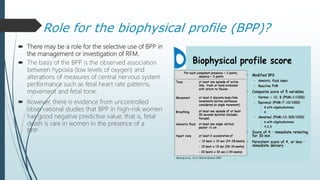
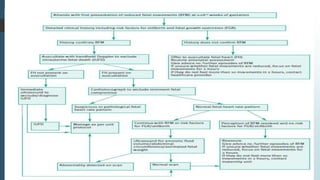
Reduced fetal movements affect 5-15% of pregnancies and women should contact their medical provider if they experience a reduction in movements after 28 weeks of gestation. A number of factors can influence a woman's perception of fetal movements. Evaluation of reduced fetal movements includes assessing the fetal heart rate with Doppler, fetal growth with ultrasound, and biophysical profile in high-risk cases. Recurrent reduced fetal movements or risk factors may warrant increased surveillance with non-stress tests and ultrasounds. Management depends on gestational age and other risk factors.