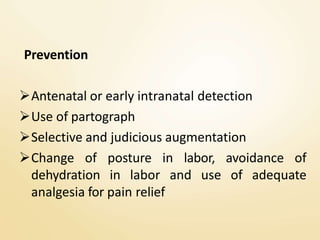
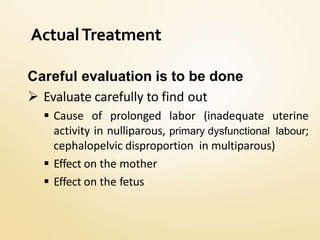
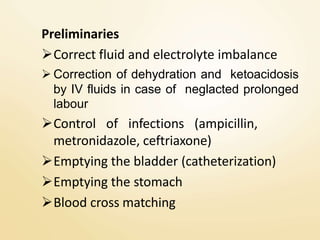
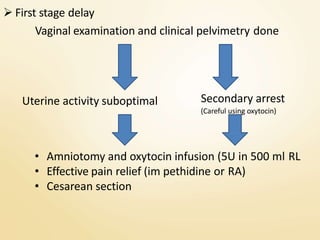
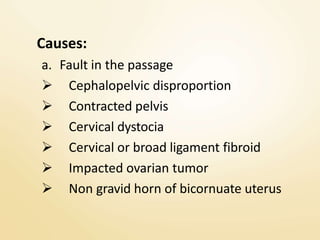
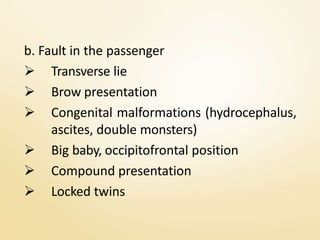
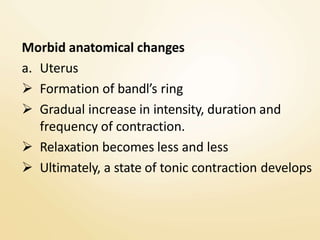
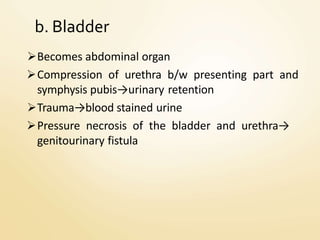
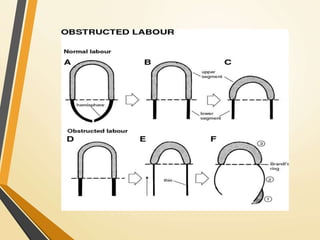
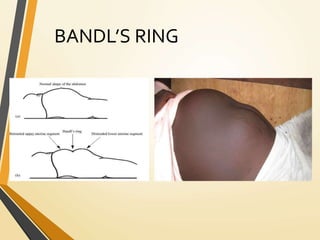
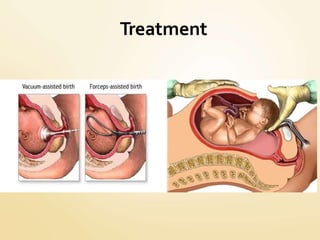
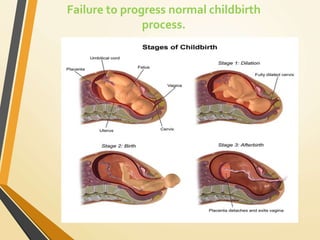
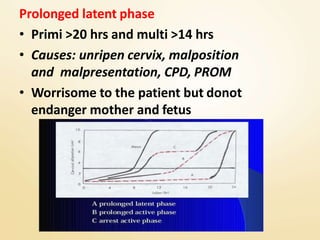
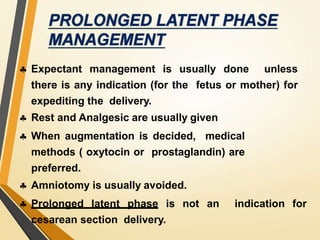
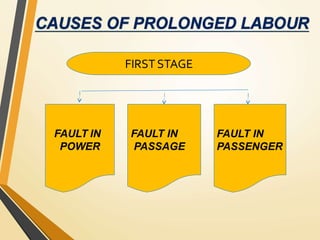
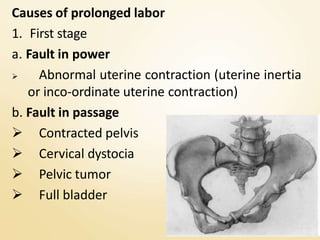
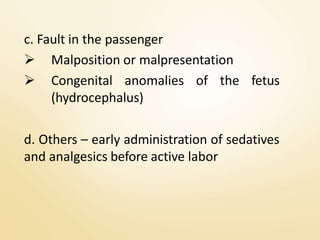
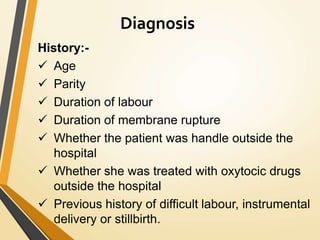
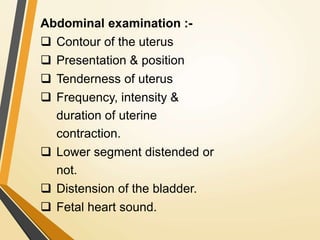
This document describes prolonged and obstructed labor. It defines prolonged labor as when the first and second stages of labor last more than 18 hours total. Obstructed labor occurs when there is poor or no progress despite strong contractions, usually due to issues with the fetus (fault in passenger) or birth canal (fault in passage). Causes include cephalopelvic disproportion, malpositions, big baby, or contracted pelvis. Diagnosis involves assessing cervical dilation rate and fetal descent rate with a partograph. Treatment depends on the stage of labor affected and may include oxytocics, analgesics, assisted delivery, or C-section. Complications can be serious for both mother and baby if not resolved.
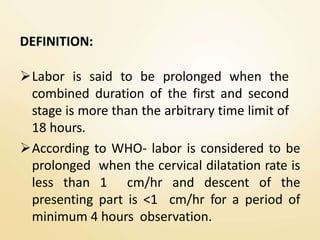
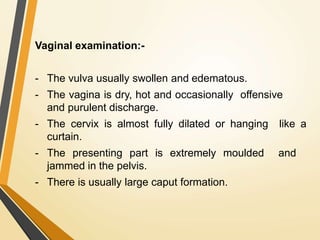
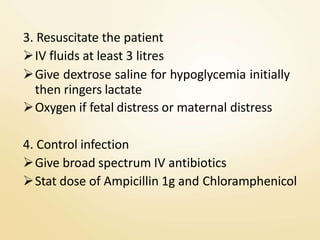
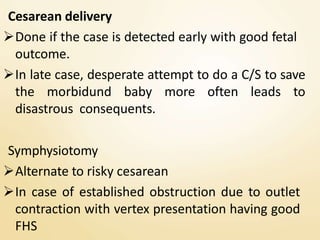
![FIRST STAGE
Duration is > 12 hours
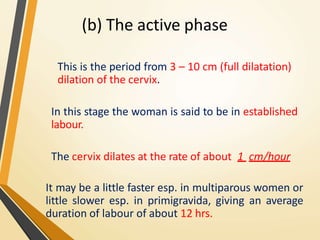
Cervical dilatation rate < 1 cm/hr in primi and
< 1.5 cm/hr
Rate of descent of presenting part is < 1 cm/hr
in primi and < 2 cm/hr in multi
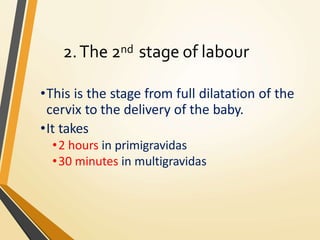
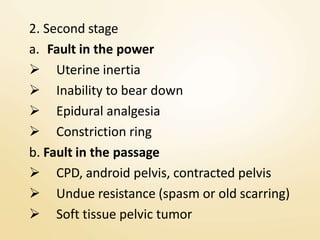
SECOND STAGE
Duration >2 hrs (nullipara), >1 hr (multipara)
[if regional analgesia is given then one hour is
permitted in both groups]](https://image.slidesharecdn.com/prolongedobstructedlabour-201130101941/85/Prolonged-and-obstructed-labour-28-320.jpg)