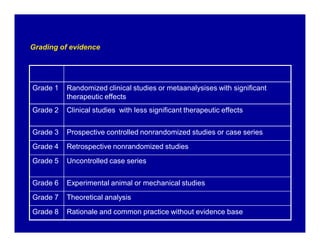
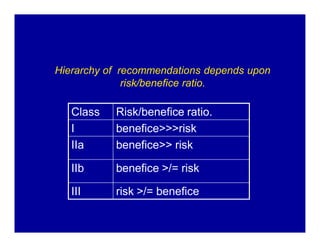
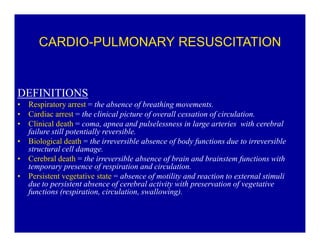
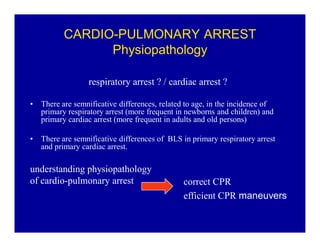
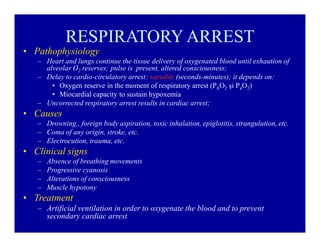
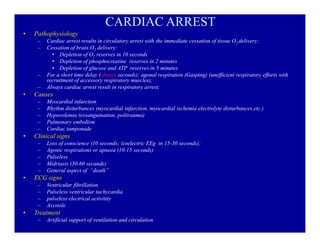
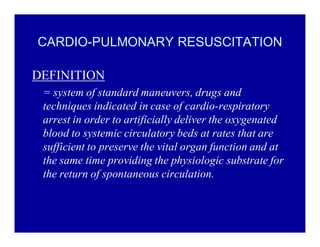
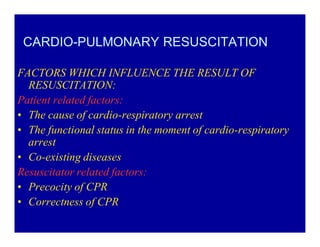
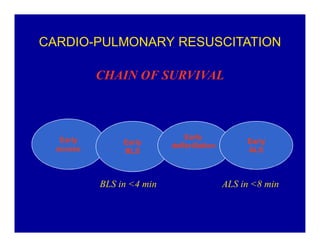
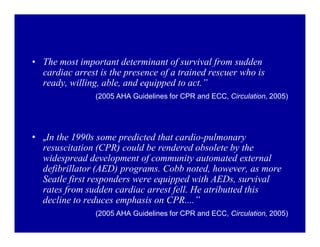
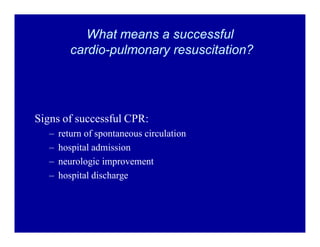
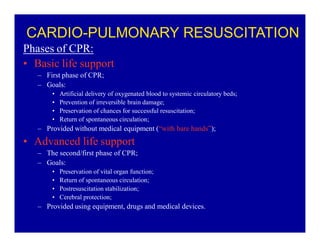
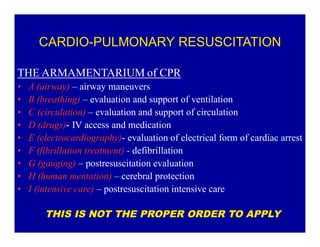
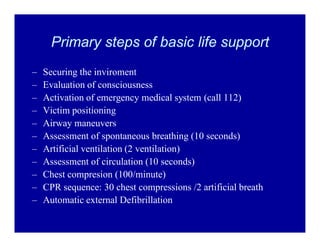
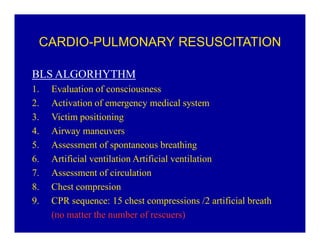
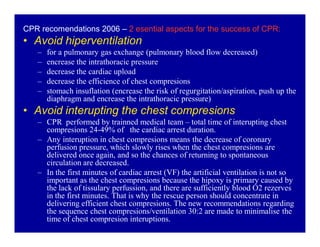
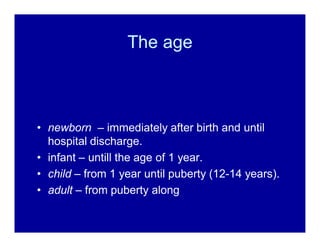
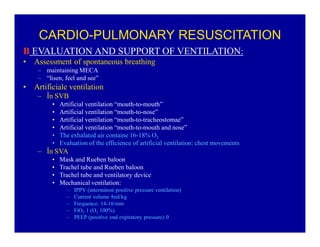
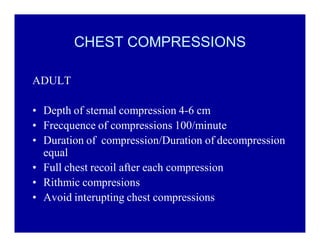
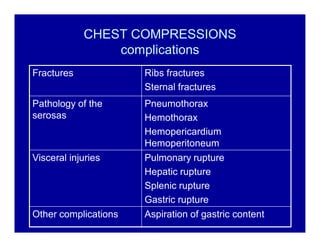
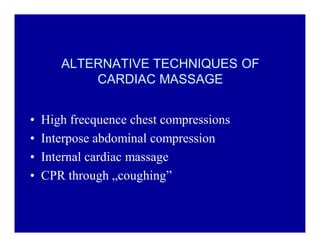
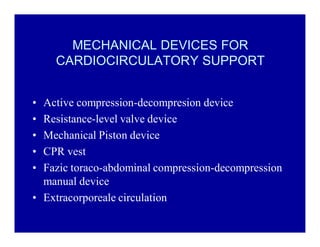
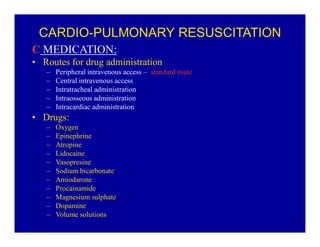
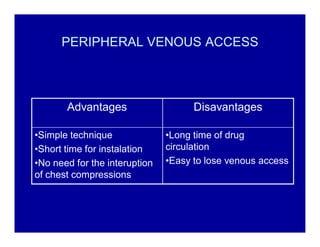
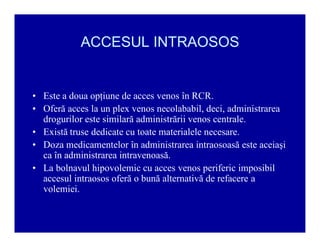
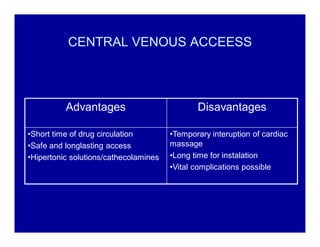
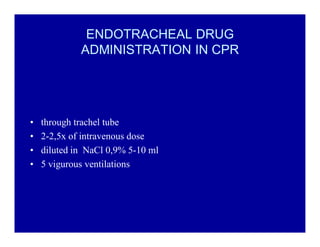
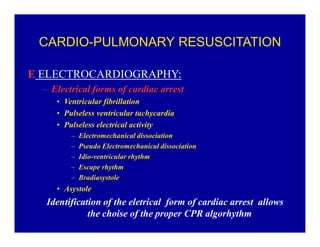
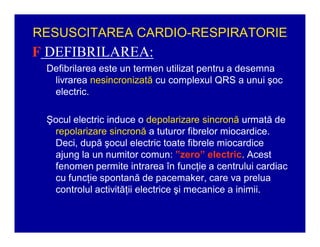
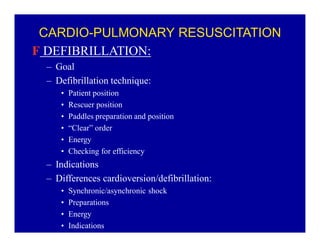
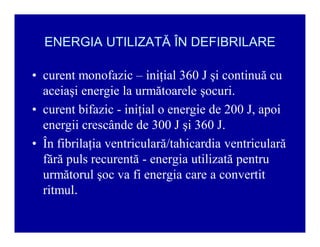
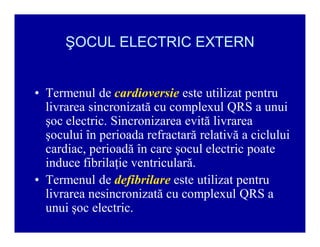
The document provides guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care, including definitions of terms, the pathophysiology and treatment of respiratory and cardiac arrest, indications for CPR, the components and steps of basic and advanced life support, airway management, ventilation, circulation support, and factors that influence the outcome of resuscitation. It establishes evidence-based recommendations to optimize CPR performance and improve survival from sudden cardiac arrest.