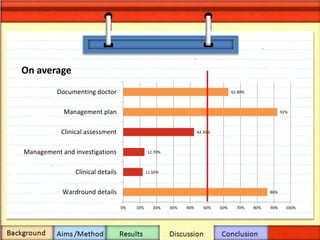
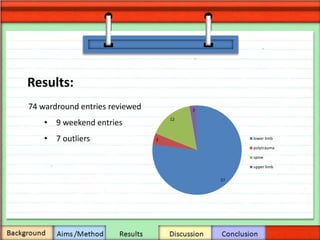
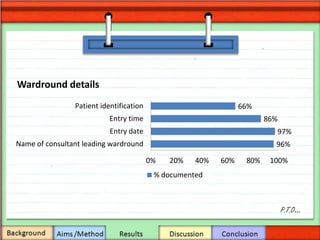
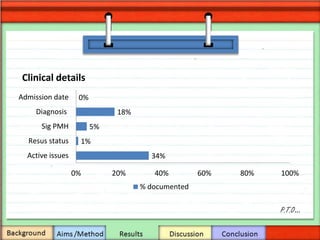
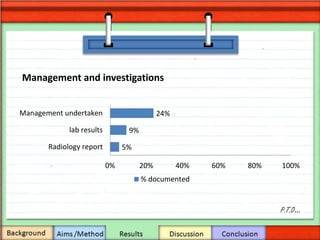
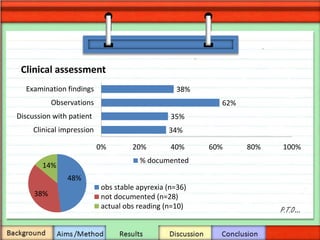
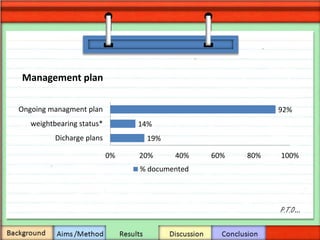
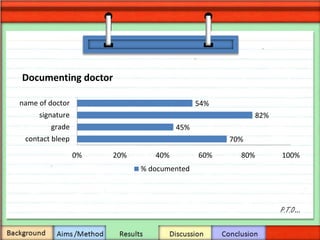
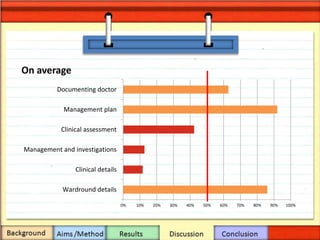
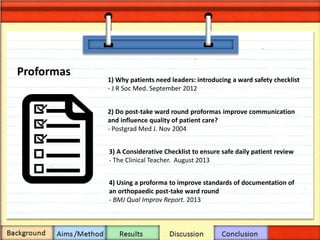
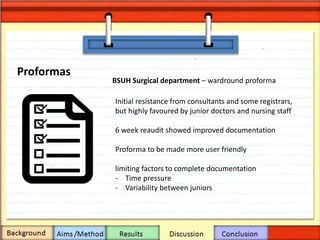
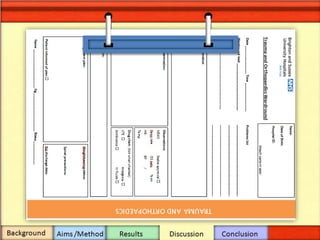
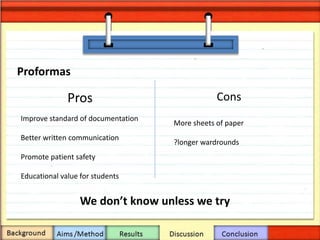
This document summarizes a ward round documentation audit conducted over 8 weeks. The results showed substandard documentation across several categories assessed. Discussion notes that poor documentation can negatively impact patient safety and care continuity. While electronic documentation may be ideal, pragmatic first steps include education, improving note access, utilizing ward round checklists, and addressing time pressures faced by junior doctors. The conclusion is that a multidisciplinary team approach is needed to implement stepwise improvements to documentation standards.