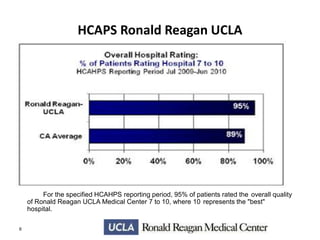
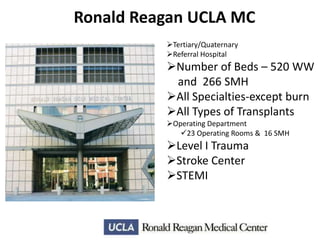
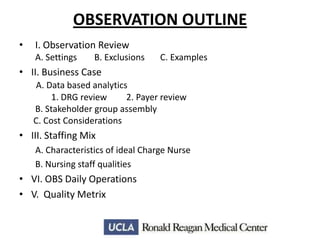
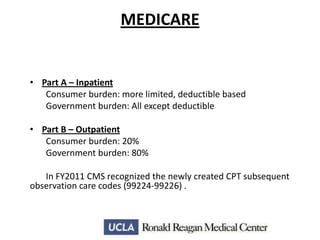
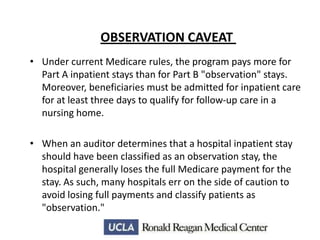
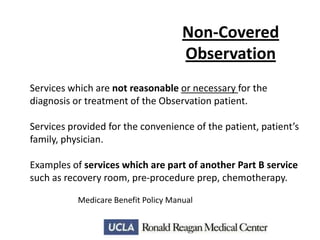
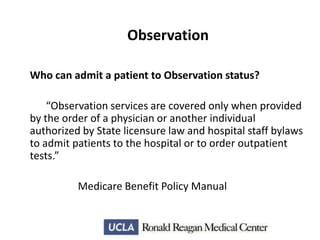
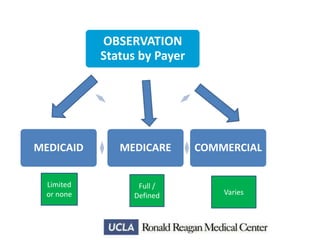
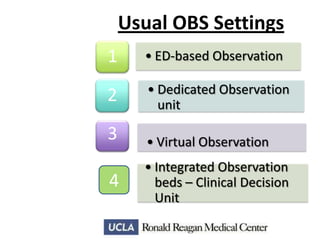
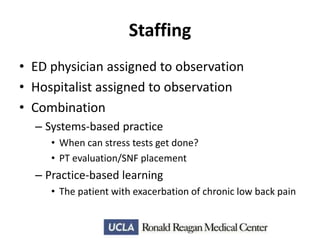
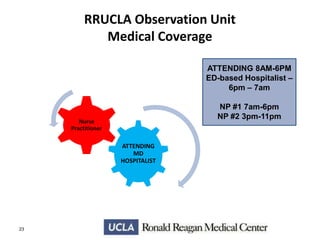
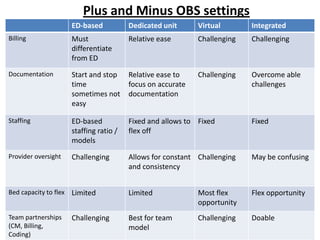
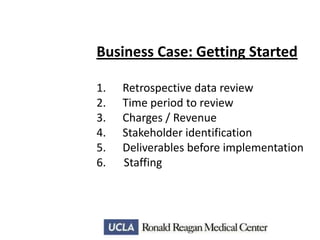
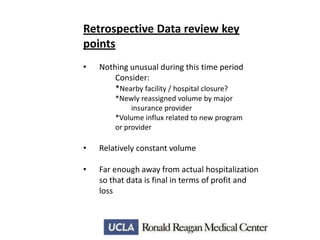
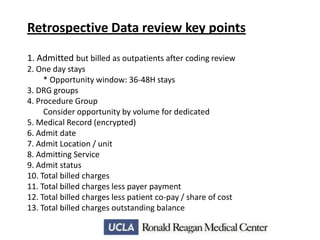
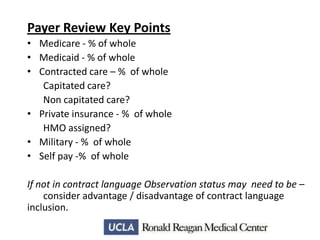
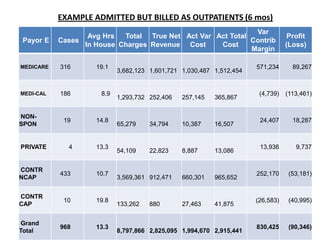
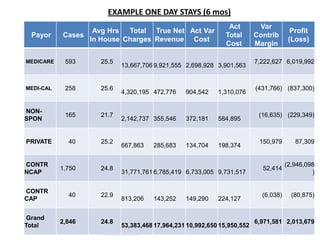
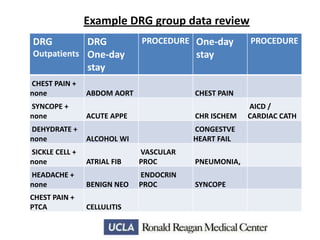
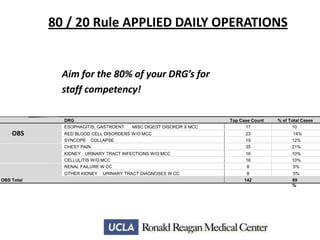
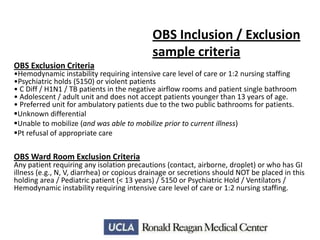
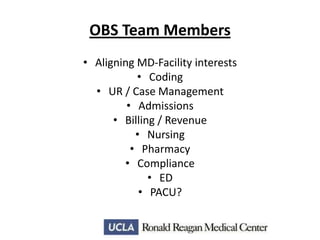
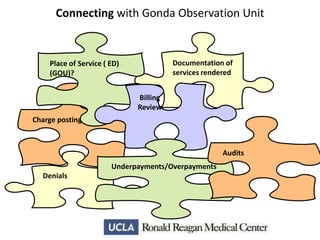
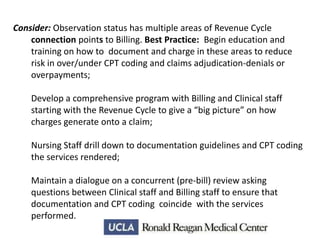
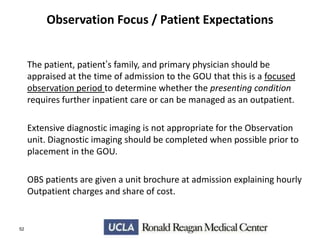
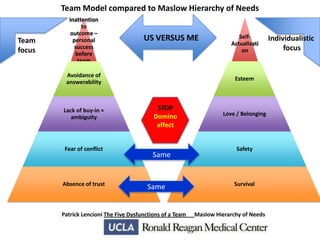
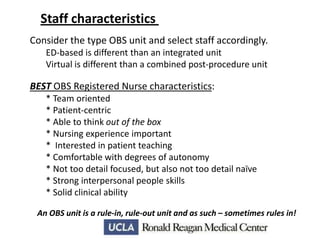
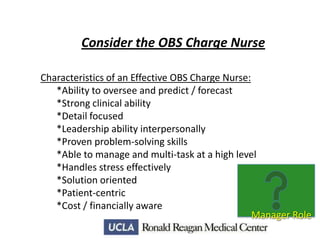
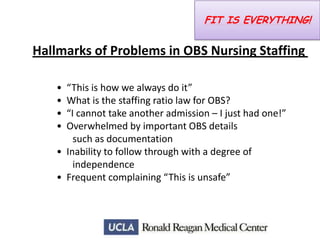
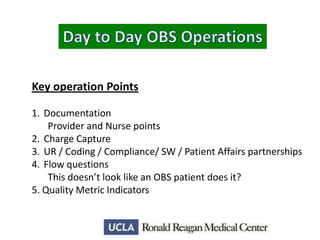
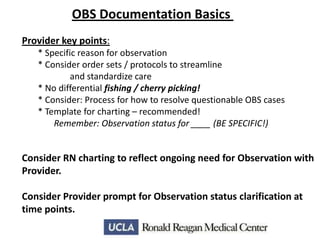
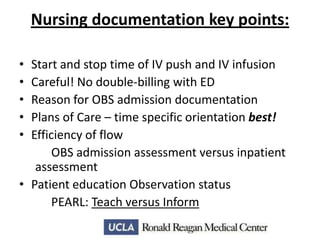
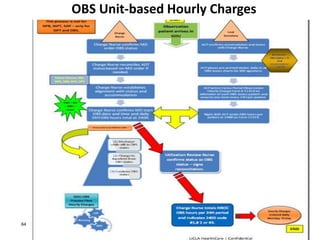
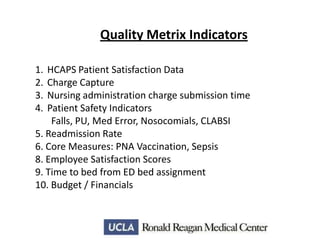
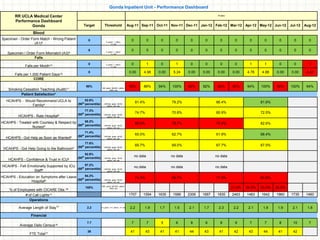
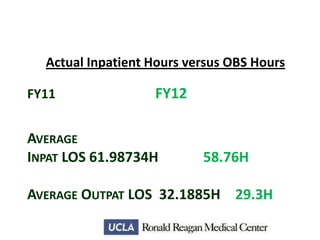
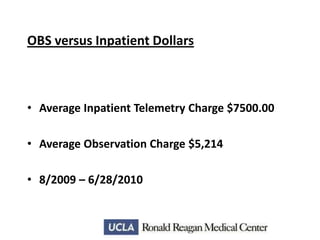
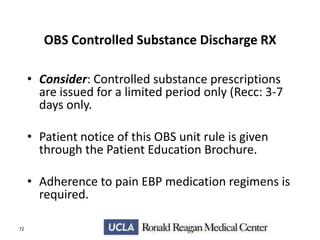
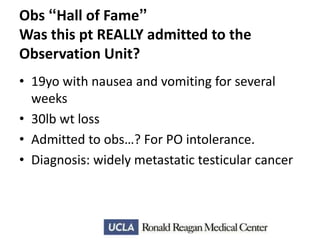
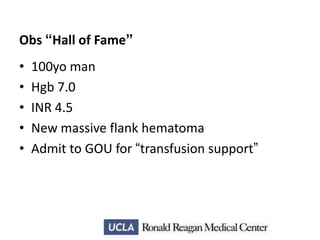
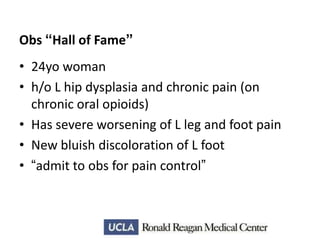
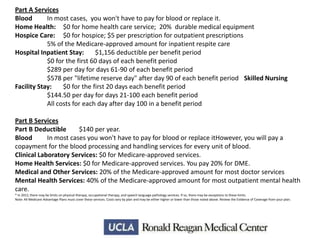
This document provides an overview and outline of topics related to observation medicine and nursing considerations at Ronald Reagan UCLA Medical Center. It discusses UCLA Health System and patient satisfaction scores. The outline covers observation review settings and examples, the business case for observation including data analysis and cost considerations, staffing mix and characteristics, daily operations, and quality metrics. It provides details on Medicare rules and coverage for observation, examples of retrospective data reviews for observation opportunities, and considerations for staffing and managing observation patients.