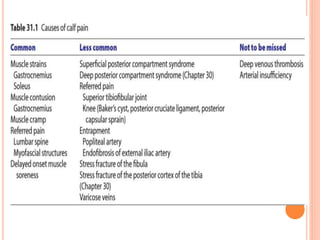
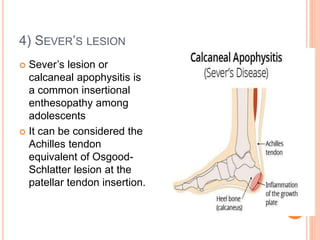
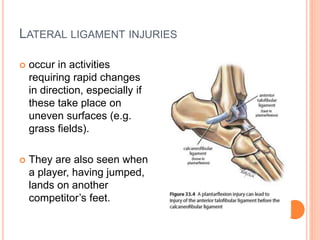
1. The document discusses various injuries to the calf and ankle, including gastrocnemius muscle strains, soleus muscle strains, Achilles tendon ruptures, Sever's lesion, and lateral and medial ligament injuries.
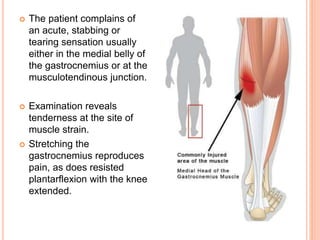
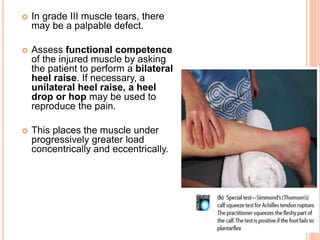
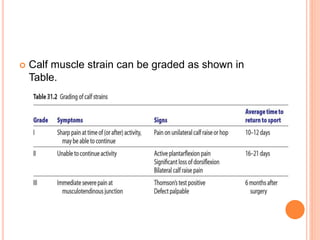
2. It describes the mechanisms, symptoms, and physical exam findings for each injury. Gastrocnemius strains typically occur during plantarflexion while soleus strains have a history of increasing tightness.
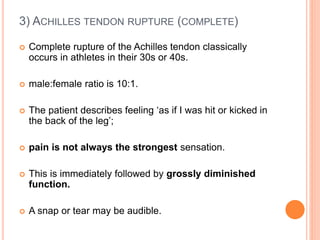
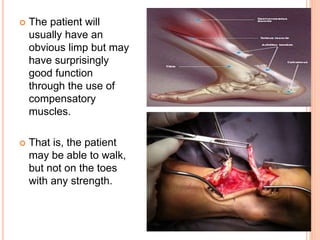
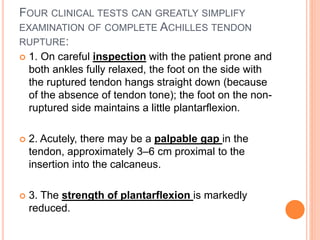
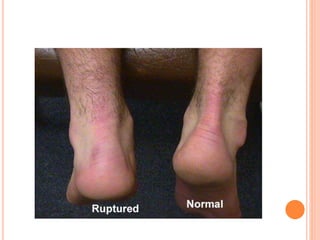
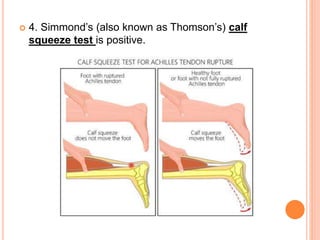
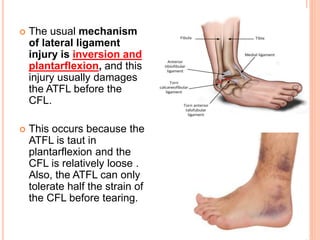
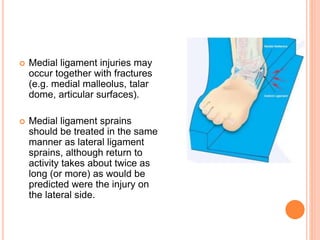
3. Achilles tendon ruptures result in a palpable gap and reduced plantarflexion strength. Ligament injuries involve inversion or eversion strains and medial injuries have a longer recovery time.