This document provides information on exercise stress testing, including:
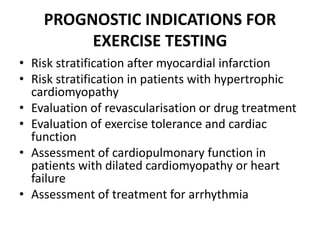
1. It describes exercise stress testing as a diagnostic and prognostic tool for assessing patients with suspected or known ischemic heart disease by evaluating their heart's response to increased metabolic demands during exercise.
2. It outlines the clinical relevance of exercise stress testing for evaluating patients with chest pain or known heart disease and notes sensitivity of 78% and specificity of 70% for detecting coronary artery disease.
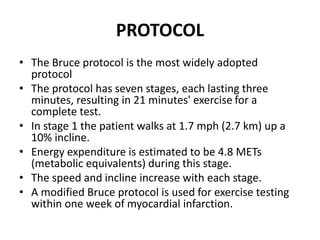
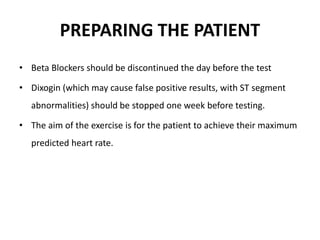
3. It discusses protocols, safety considerations, electrocardiographic changes monitored, and contraindications for exercise stress testing.