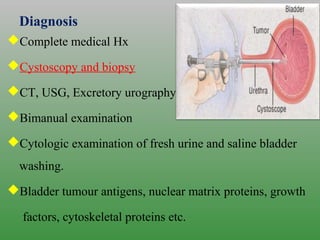
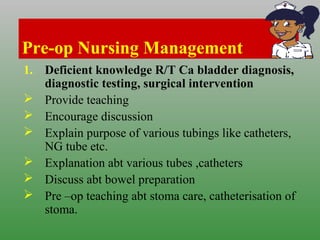
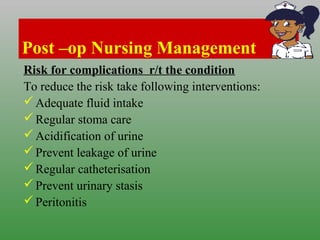
This document discusses carcinoma of the bladder. It begins by defining bladder cancer and noting that it forms in bladder tissues and may infiltrate the bladder wall. It then covers the epidemiology, risk factors, pathophysiology, types, clinical manifestations, staging, grading, diagnosis and management of bladder cancer. Management includes surgery such as TURBT and cystectomy, chemotherapy, radiation therapy, and intravesical drug therapy. Nursing management involves assessment, education, managing anxiety and pain, and monitoring the urinary drainage system after any procedures.