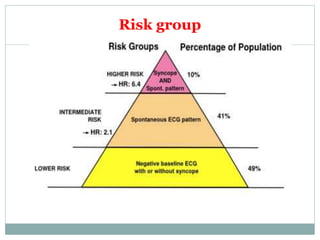
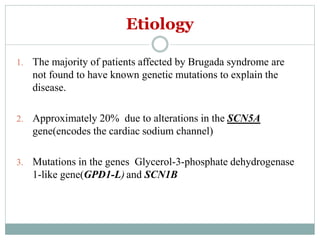
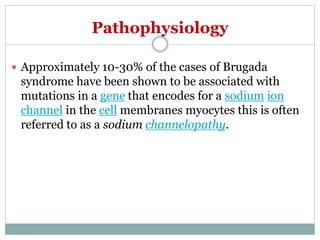
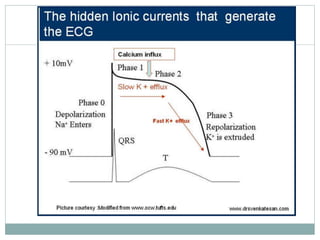
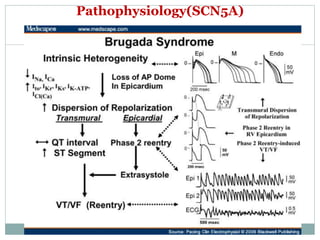
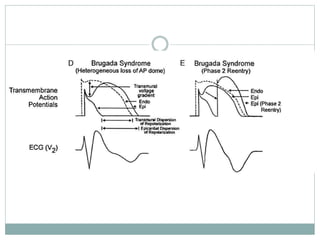
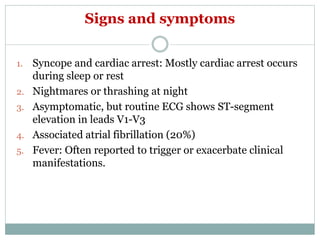
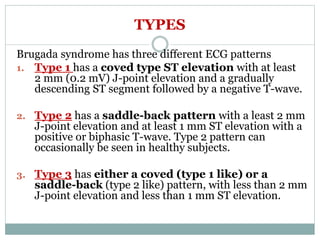
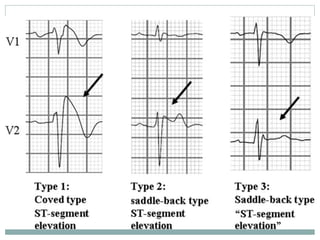
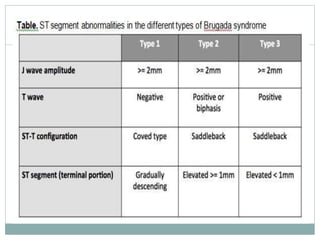
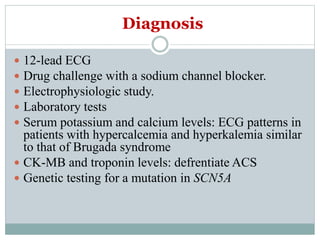
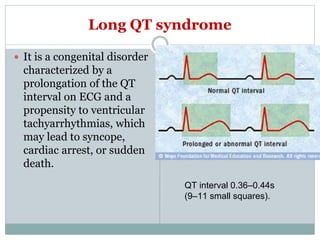
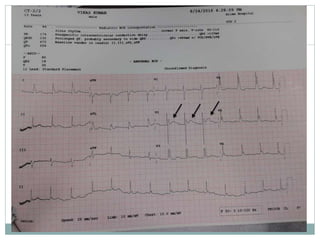
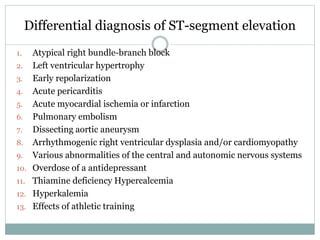
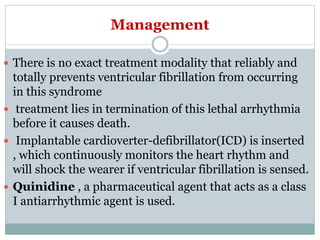
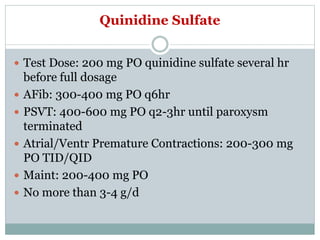
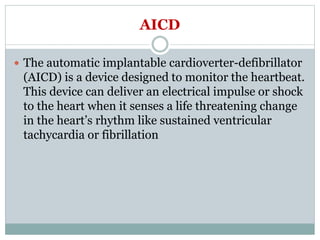
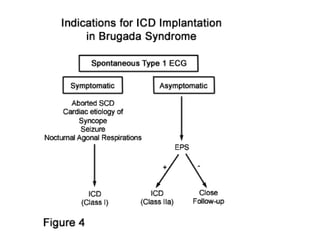
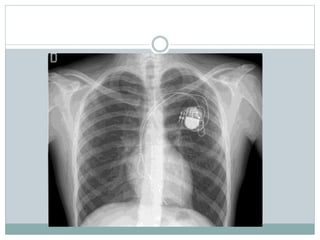
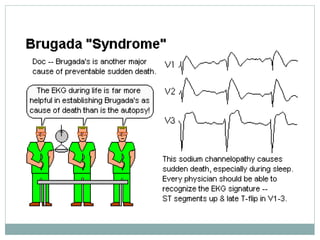
Brugada syndrome is a genetic heart condition characterized by abnormal ECG patterns and risk of sudden cardiac death. It is caused by mutations in genes encoding sodium channels. The condition is diagnosed through ECG showing ST segment elevation in leads V1-V3. Treatment involves implanting an ICD to detect and treat lethal arrhythmias with shocks. Prognosis depends on risk stratification and treatment.