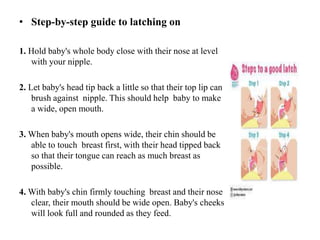
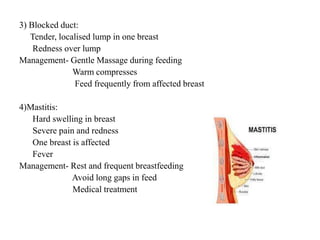
The document discusses the significance of breastfeeding, including its health benefits, hormonal mechanisms, and composition. It outlines the proper techniques for latching and signs of effective and ineffective suckling, as well as contraindications to breastfeeding under certain conditions. It also presents guidelines and steps for successful breastfeeding practices, addressing challenges that may arise in specific situations such as low birth weight and maternal health issues.