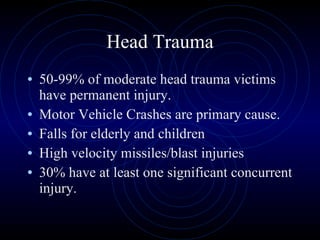
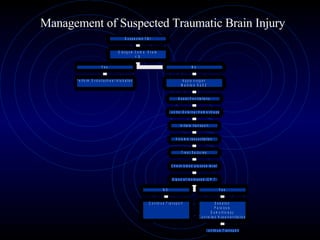
1) Head trauma can cause permanent injury, with motor vehicle crashes and falls being common causes. Approximately 30% of those with moderate head trauma have at least one other significant concurrent injury.
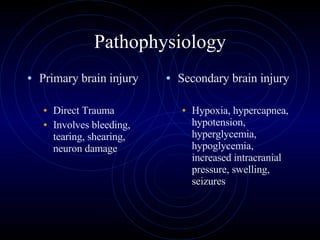
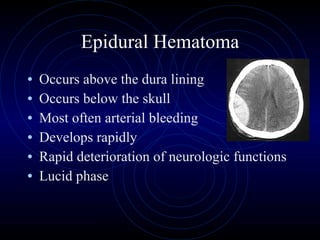
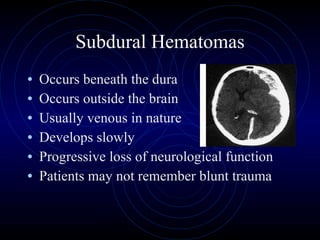
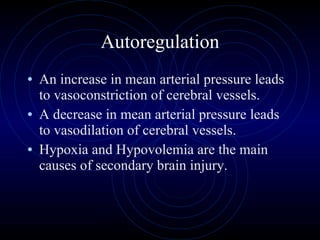
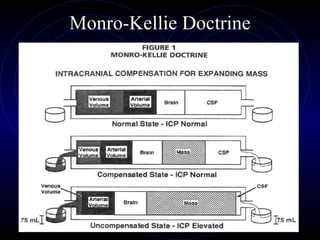
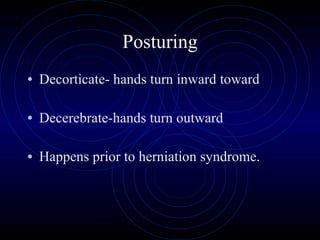
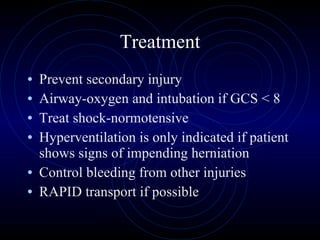
2) Primary brain injury results directly from trauma and causes bleeding, tearing and shearing of brain tissue. Secondary brain injury can occur later and includes hypoxia, swelling and increased pressure inside the skull.
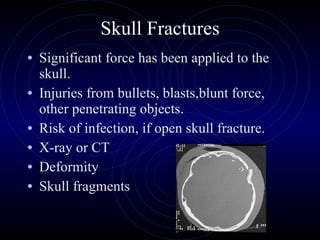
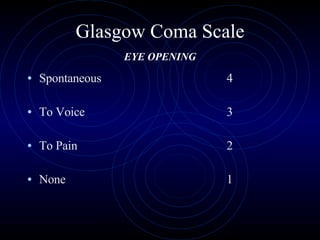
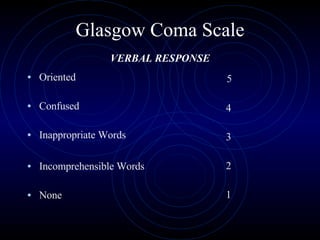
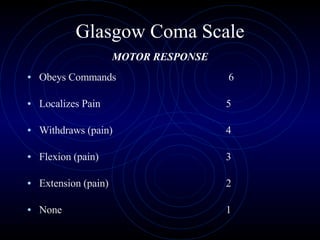
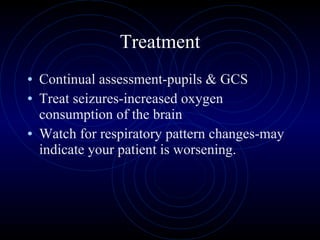
3) Various types of head injuries are discussed, including scalp lacerations, skull fractures, concussions, contusions and bleeding within or around the brain. The Glasgow Coma Scale is used to assess level of consciousness.