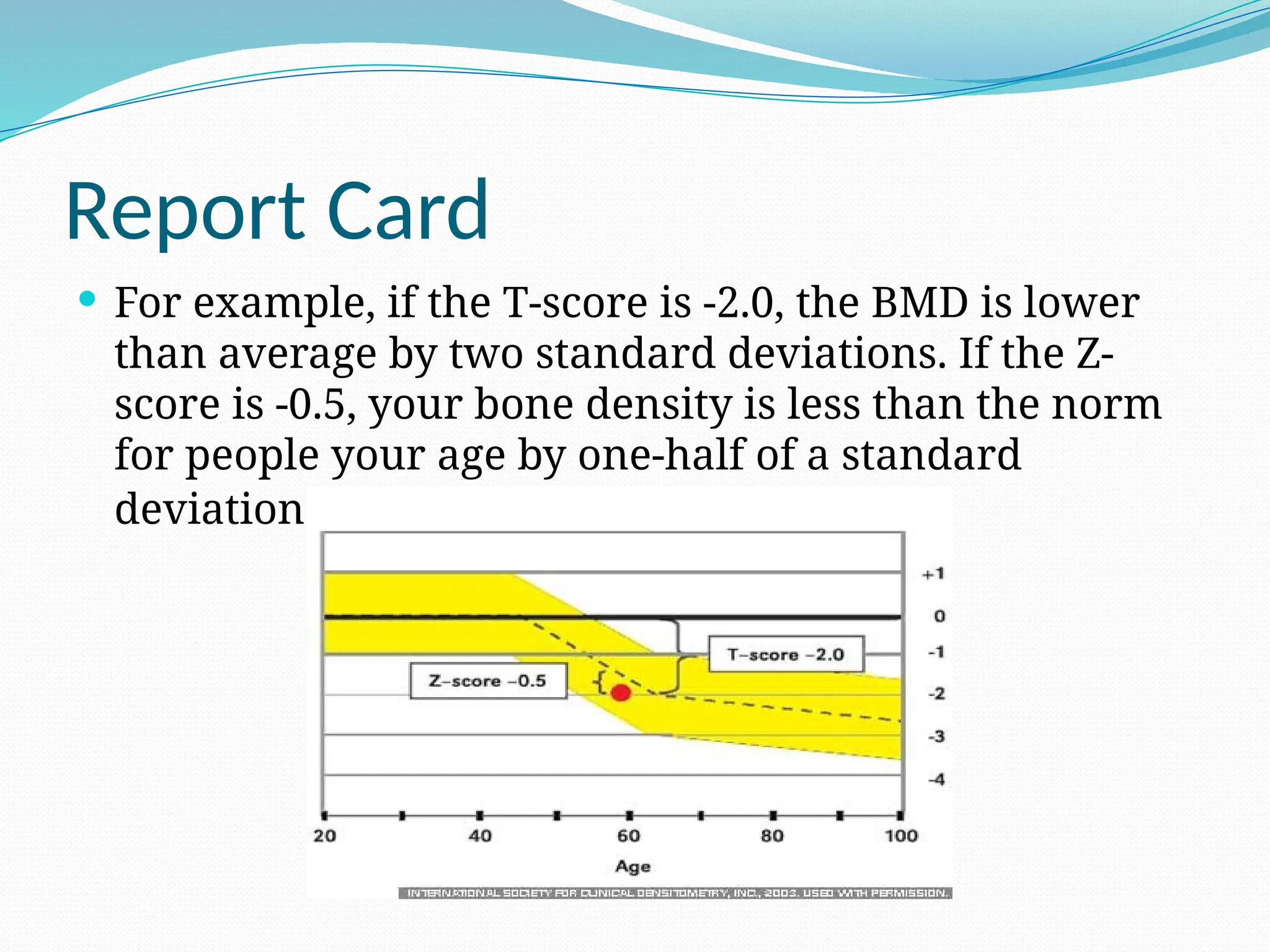
The document provides an overview of osteoporosis, a condition characterized by decreased bone mass and increased fracture risk, and outlines demographics for bone mineral density (BMD) testing, including postmenopausal women and men with fractures. It discusses various diagnostic techniques, notably dual-energy X-ray absorptiometry (DXA), and emphasizes the importance of screening and monitoring bone health, particularly in vulnerable populations. The document also highlights the limitations and preparation requirements for BMD tests, alongside the utility of additional imaging methods such as quantitative computed tomography and ultrasound densitometry.