Oncology imaging
- 2. INTRODUCTION Advances in diagnostic imaging have increased our ability to visualize macroscopic disease, referred to as gross tumor volume (GTV). Imaging is currently unable to identify microscopic tumor extension around a primary tumor or occult nodal involvement.
- 3. • Radiation treatment planning has undergone considerable evolution during the past 20 years. • With conventional planning, the physician conceives of beam orientations and aperture shapes based on the interpretation of clinical and diagnostic information, including three-dimensional (3D) imaging data such as computed tomography (CT) or magnetic resonance imaging (MRI).
- 4. • Radiologic imaging is an integral component in the management of cancer patients. • Imaging is utilized in the diagnosis and initial staging of disease, treatment planning, and posttreatment Surveillance. • A general sense of the sensitivity, specificity, and positive and negative predictive values of an imaging study helps the clinician assimilate and interpret imaging information that can be misleading or even contradictory.
- 5. RADIOGRAPHY Conventional radiography creates a two-dimensional grayscale image produced by the differential attenuation of x-rays that pass through soft tissues of varying density. Tissues that are very dense, such as bone, will absorb more x-rays than tissues that are less dense, such as lung.
- 6. • Radiographs are therefore best suited to detect pathology when a lesion differs greatly in density from adjacent structures, such as a soft tissue mass surrounded by aerated lung or a lytic lesion surrounded by dense bone. • Radiographs have excellent spatial resolution: the ability to detect a small object within a given volume. However, they are suboptimal when there are only subtle differences in tissue density. • Therefore, even large lesions can be missed if they are of similar density to surrounding structures.
- 7. CT, MRI, and ultrasound (US) generate two-dimensional cross-sectional images. The benefits of cross-sectional imaging include visualization of superimposed structures obscured on planar images, improved anatomic detail of individual organs and their precise relationship to adjacent structures, and the ability to perform multiplanar reconstructions. Furthermore, some applications provide functional in addition to morphologic information and can be acquired in real time, permitting image guidance for procedures. For these reasons, cross-sectional modalities are the mainstay of oncologic imaging.
- 8. CROSS SECTIONAL IMAGING Computed Tomography (CT) Magnetic Resonance Imaging (MRI) Ultrasound (US)
- 9. COMPUTED TOMOGRAPHY • CT generates cross-sectional images from the transmission of radiation through tissue. A patient lies on the scanner table within a gantry that houses an x-ray generator opposite multiple rows of detectors, hence the term multidetector CT (MDCT). • Current generation scanners (e.g., 64 or 128 MDCT) are able to acquire high- resolution image data much faster due to improvements in the number of detectors and computer processing. • As the gantry rotates, the detectors measure x-ray transmission through the rotation, or slice. The patient is moved through the scanner as the gantry rotates, resulting in a helical or spiral course at a very thin slice thickness, typically 0.625 mm.
- 10. The spatial and temporal data from multiple projections are then processed by a Fourier transform mechanism generating two- dimensional axial images. The thin-slice volume dataset is isotropic, meaning that images can be reconstructed in orthogonal and oblique planes without a loss in image quality. Furthermore, thin-slice acquisition improves contrast resolution and decreases partial volume artifacts, thereby improving imaging quality and accuracy. Images are displayed within a matrix composed of voxels, each representing a volume of radiodensity that is quantified by a linear attenuation value called a Hounsfield unit (HU).
- 11. Each voxel is assigned a HU in the range of –1,000 to 1,000 corresponding to a shade of gray to represent the attenuation difference between a given material and water. By convention, air is the least dense material with a HU value of –1,000, while water has a HU value of 0. Soft tissues have a range of attenuation with typical HU values as follows: fat (–120), blood (30), muscle (40), bone (>300). HU analysis is more accurate than visual assessment of tissue composition and is particularly useful in characterizing enhancement postcontrast administration, a feature critical in the assessment of many solid organ lesions.
- 12. • Both intravenous (IV) and oral contrast agents may be utilized to improve spatial resolution. Oral contrast agents are routinely used for abdominal and pelvic imaging to distinguish bowel from adjacent organs, lymph nodes, and tumors. • The use of an intravascular contrast agent during CT depends on the study indication, target organ, and patient status. • Administration of IV contrast media is required for thorough assessment of vessels (e.g., aorta, pulmonary arteries), solid organs (e.g., liver, kidneys), and characterization of lesion vascularity.
- 13. • Contrast-enhanced CT is often necessary to detect solid organ metastases (e.g., liver, adrenal gland, brain). Contrast is usually not necessary for routine pulmonary imaging due to the inherent contrast of solid lesions within a background of aerated lung, although it does improve the characterization of hilar lymph nodes.
- 14. • Given that the administration of contrast media can alter tissue attenuation, the HU value of a lesion or tissue may differ depending on whether the study was performed with or without contrast and based on the timing of image acquisition (e.g., arterial vs. portal venous phase). • HUs are used during radiation treatment planning dose calculations; therefore, contrast can affect these calculations. • If indicated, the HU within a structure enhanced by contrast (e.g., the bladder when planning for prostate cancer treatment) can be set to an alternate value prior to dose calculations.
- 15. • A similar phenomenon often occurs when materials with a high atomic number are within the scanned volume. • These materials (e.g., dental fillings, hip prostheses) can cause artifacts that can make it challenging to accurately segment the image or affect dose calculations. The latter can also be corrected by setting the HU within the affected area to the desired value.
- 16. MAGNETIC RESONANCE IMAGING • MRI generates cross-sectional images without ionizing radiation. • MRI utilizes strong magnets, typically 1.5 or 3.0 T for clinical applications. • A 3.0 T magnet is 60,000 times greater than the earth’s magnetic field. • The magnetic field uniformly aligns the nuclei of hydrogen protons within tissue. • Applying a radiofrequency (RF) pulse sequence and gradient to the magnetic field disrupts this alignment and equilibrium. • When the RF pulse is removed, the protons realign, or relax, within the field and emit a measurable resonance radio signal. The detected radio signals, referred to as echoes or spin echoes, are then used to generate an image.
- 17. • The most important tissue properties for image generation are the proton density, the spin-lattice relaxation time (T1) and the spin-spin relaxation time (T2). • Different tissues have different proton density and relaxation times, absorbing and releasing radio wave energy at different rates, which in part accounts for the high tissue contrast obtained by MRI. • Different RF pulse sequences can accentuate different tissue characteristics by varying parameters such as the repetition time (TR)—the time between RF pulses in the sequence, which determines how much time protons have to realign within the magnetic field—and the echo time (TE)—the time between the RF pulse and the peak returning signal.
- 18. • TR and TE dramatically affect image contrast and determine which tissue properties are selected. • T1-weighted images, in which fluid is dark and fat is bright, are generally good at depicting anatomy; • T1-weighted images are generated by selecting short TR (typically ≤800 ms) and short TE values (≤30 ms). • T2-weighted images, in which fluid is bright and fat is dark, are fluid-sensitive and can depict areas of pathology; • T2-weighted images are generated by selecting long TR (≥2,000 ms) and long TE values (≥60 ms).
- 19. • Gadolinium chelates are the most commonly used MRI contrast agents, which, like the iodinated CT equivalents, are confined to the vasculature and do not cross an intact blood– brain barrier. • Gadolinium-based contrast media are at increased risk of developing NSF. • One of the advantages of MRI over CT is that it can provide functional in addition to anatomic information. • This is particularly beneficial in oncologic imaging. MRI techniques allow for tissue diffusion and perfusion imaging, quantification of blood flow by velocity phase encoding, and magnetic resonance proton spectroscopy, which provides biochemical quantification of tissues.
- 20. PRECAUTIONS • MRI has modality-specific artifacts that can limit image quality. Motion artifact can be problematic with MRI due to long scan times. • Chemical shift artifact results in a loss of signal at the interface of tissues with highly variable contrast properties. • MRI is also highly sensitive to magnetic field distortions that can produce artifacts. • Patients must be carefully screened to ensure that any medical devices or surgical hardware are MRI compliant.
- 21. ULTRASONOGRAPHY • US is an imaging modality utilizing pulse-echo techniques rather than radiation to produce an image. • The US transducer coverts electrical energy into a high- frequency pulse that is transmitted through tissues. • The pulse interacts at tissue interfaces, generating a reflected echo signal that is detected by the transducer. • The returning sound waves are transformed into a gray scale image in real time. Image quality is, in large part, determined by the pulse frequency. High-frequency transducers
- 22. • (5–12 MHz) produce high-resolution images but have limited ability to penetrate. Therefore, they are best suited to imaging superficial structures such as the breast or thyroid. • Low frequency transducers (1–3.5 MHz) generate lower quality images but have better tissue penetration and are most often used for imaging abdominal and pelvic organs. • The degree to which tissues are visualized by US is called echogenicity. Fat is highly echogenic (bright), whereas fluid-containing structures, such as simple cysts, are anechoic (dark).
- 23. COLOR DOPPLER • Color Doppler US is an important adjunct to conventional gray-scale sonography. • The Doppler effect is a change in frequency of returning sound waves reflected by a moving object, such as flowing blood. • If blood flows away from the transducer, the echo frequency decreases; whereas if blood flows toward the transducer, the echo frequency increases. • The change in frequency is directly proportional to the flow velocity and produces a color overlay in areas of flow on the standard gray-scale US image. • Color Doppler US is useful in characterizing blood flow within lesions and assisting in image-guided procedures.
- 24. ENDOSCOPIC ULTRASOUND • Endoscopic ultrasound (EUS) was introduced in the early 1980 s and has become a tool important in oncologic staging. • It allows for high-resolution images of internal structures not typically accessible by high-frequency transducers by passing the probe through bowel or airways. • It is most widely applied in the setting of gastrointestinal (GI) malignancies, especially esophageal and rectal carcinomas. • A 5 to 12 MHz transducer can readily identify five of the layers of the gastrointestinal tract. Higher frequency transducers can identify additional layers, such as the muscularis mucosa and lamina propria of the esophagus, which has important staging implications.
- 25. • EUS is also utilized for characterization and image-guided sampling of regional lymph nodes in GI or bronchopulmonary disease. The ability of EUS to predict the tumor (T) stage is generally superior to its ability to predict the node (N) stage. • Suspicious lymph nodes are typically round, >10 mm in short axis, have distinct margins, and are typically hypoechoic. If all four features are present, the likelihood of malignancy is 80% to 100%. There is, however, considerable overlap between benign and malignant features of lymph nodes on EUS in addition to wide inter-observer variability. • Tissue sampling is therefore recommended for accurate staging. When describing clinical T and N staging by EUS, the prefix u should be utilized (e.g., uT3N1).
- 26. AXIAL ENDOSCOPIC ULTRASOUND IMAGE (RIGHT) AND HISTOLOGIC SPECIMEN (LEFT) FROM A NORMAL ESOPHAGUS. THE ENDOSCOPIC ULTRASOUND LAYERS AND HISTOLOGIC LAYERS OF THE ESOPHAGUS ARE CORRELATED (SEE TABLE 30.3). (ENDOSCOPIC ULTRASOUND IMAGE COURTESY OF DR. F RANK GRESS. H ISTOLOGIC IMAGE COURTESY OF DR. DANIEL GOODENOUGH.)
- 27. NUCLEAR IMAGING Positron Emission Tomography Bone Scintigraphy
- 28. INTRODUCTION • Although radiographic and cross-sectional studies provide important anatomic information regarding pathologic processes, nuclear radiology provides physiologic information based on the distribution of an injected or ingested radiopharmaceutical. • Radiopharmaceuticals consist of a radioactive substrate (radionuclide, radioisotope, or radiotracer) that is coupled with a physiologically active compound or analog. For example, technetium-99 m is a radioisotope that is coupled to pertechnetate, an iodine analog, which can enter thyroid follicular cells. • The timing of imaging depends on the kinetics of absorption, metabolism, and half- life of the radionuclide. Gamma rays emitted by nuclear decay of the radionuclide are then detected using a γ-camera corresponding to radiotracer activity that is described in terms of uptake. • Indium-111 capromab pendetide (ProstaScint) can be utilized for prostate cancer and gallium-67 can be used for lymphomas.
- 29. POSITRON EMISSION TOMOGRAPHY • Although several radionuclides for PET are available, the most common is 18-fluorodeoxyglucose (FDG). • FDG is a glucose analog that concentrates in areas of high metabolic activity. Tumor cells are often highly metabolic, with rapid cell division and an increased number of glucose transporters. • However, FDG uptake is not specific for malignancy and accumulates in any cell with increased metabolic activity, including myocardium, gastric mucosa, brain tissue, thyroid, and salivary glands, which limits evaluation of these organs. 2
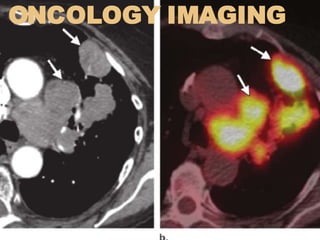
- 30. • Furthermore, FDG tracer is excreted within the urinary system; therefore, activity within the kidneys, collecting system, and bladder can obscure malignancy of these structures. • Notwithstanding these limitations, PET-CT has become the preferred imaging modality for clinical staging, facilitating the characterization of benign versus malignant pathology, detecting sites of unsuspected disease, identifying optimal sites for tissue sampling, assessing treatment response, and monitoring for recurrence for multiple malignancies. • PET-CT combines the physiologic assessment of PET with the anatomic assessment of CT, resulting in improved diagnostic accuracy.
- 31. • Patients must fast for 4 to 6 hours prior to scanning in order to limit metabolic activity within the GI tract. • Blood glucose levels should be well controlled (<150 mg/dL) to limit glucose receptor competition with FDG, as high glucose levels can result in a false- negative scan. • Speech and motion should be restricted to minimize muscle uptake, which could obscure pathology. • Approximately 1 hour following FDG administration, a CT scan is performed immediately followed by PET imaging, which can take up to 60 minutes. • CT and PET datasets are then reconstructed in separate axial, coronal, and sagittal series as well as fused PET-CT images.
- 32. • FDG uptake is nonspecific, localizing to any tissue with increased metabolic activity. Although most malignant tumors are hypermetabolic relative to normal tissues, non-malignant processes also concentrate FDG, including foci of infection, inflammation, and benign neoplasms. • FDG uptake is quantified by the standard uptake value (SUV). Most malignant tumors have a maximum SUV >2.5, while physiologic uptake is typically <2.5. SUVs are not absolute and can be affected by the timing of imaging, improper attenuation correction, partial volume affects, patient weight, FDG dose, and factors affecting FDG uptake. • Clinical studies to date have documented that under such uniform conditions, changes in SUV have prognostic value, indicating that most tumors responding to therapy show a 20% to 40% decrease in SUV early in course of treatment.
- 33. BONE SCINTIGRAPHY • Normal bone undergoes continuous remodeling, maintaining a delicate balance between osteoblastic and osteoclastic activity. • Most bone metastases originate as intramedullary lesions, having gained access to the bone through the vasculature. • As the lesions enlarge, reactive osteoblastic and osteoclastic changes result in characteristic radiographic changes indicative of bone metastases (sclerotic, lytic, or mixed lesions). • Rapidly growing metastases tend to produce lytic lesions, while more slowly growing metastases typically produce sclerotic (or blastic) lesions. • Metastases from multiple myeloma, thyroid cancer, and renal cell carcinoma are predominantly lytic, while blastic lesions are associated with breast and prostate cancers. • The primary utility of bone scintigraphy in oncologic imaging is the detection of osseous metastatic disease.
- 34. • Bone scintigraphy or bone scan imaging utilizes radiopharmaceuticals composed of bisphosphonates; the most common of which is the radionuclide technetium-99 m methylene diphosphonate (99mTc-MDP). • 99mTc-MDP localizes to areas of new bone mineralization, which occurs in a wide array of bone pathology and is therefore highly sensitive to osseous disease, but is not very specific. • Although a 30% to 50% reduction in bone density must occur before bone metastases are detected on radiographs, as little as 5% to 10% change is required to detect such on a bone scan. • Furthermore, bone scans are relatively inexpensive, convenient, and visualize the entire skeleton, including sites that are difficult to assess on plain films (e.g., ribs, sternum, scapula, sacrum). Reported sensitivities range from 62% to 100% with similar specificity rates (78% to 100%).18
- 35. • Two primary patterns of radiotracer activity can be associated with malignancy: increased or decreased activity. • Increased uptake occurs in areas of increased blood flow and osteoblastic activity; this is a common finding in metabolically active tumors and small sclerotic metastatic foci. • Decreased radiotracer activity occurs as a “cold” area on bone scan and is associated with lytic bone disease and aggressive tumors that outgrow their blood supply. • Rapidly progressing and purely lytic disease are the main causes of false-negative findings on bone scintigraphy, while false-positive findings can be related to trauma, healing, benign bone tumors, or arthritic changes
- 36. • Tumor response may cause a “flare phenomenon,” resulting from increased activity secondary to new osteoblastic activity concomitant with new bone formation. This may be falsely attributed to progressive disease. • Similarly, lytic lesions that were previously “cold” on bone scan can transform into “hot” spots (areas of uptake) after treatment. • Second, rapidly progressive disease with overwhelming bone destruction without new bone formation can be misinterpreted as stable or responding disease on bone scan.
- 37. Choose the most appropriate imaging modality is the key for accurate, effective diagnosis and treatment