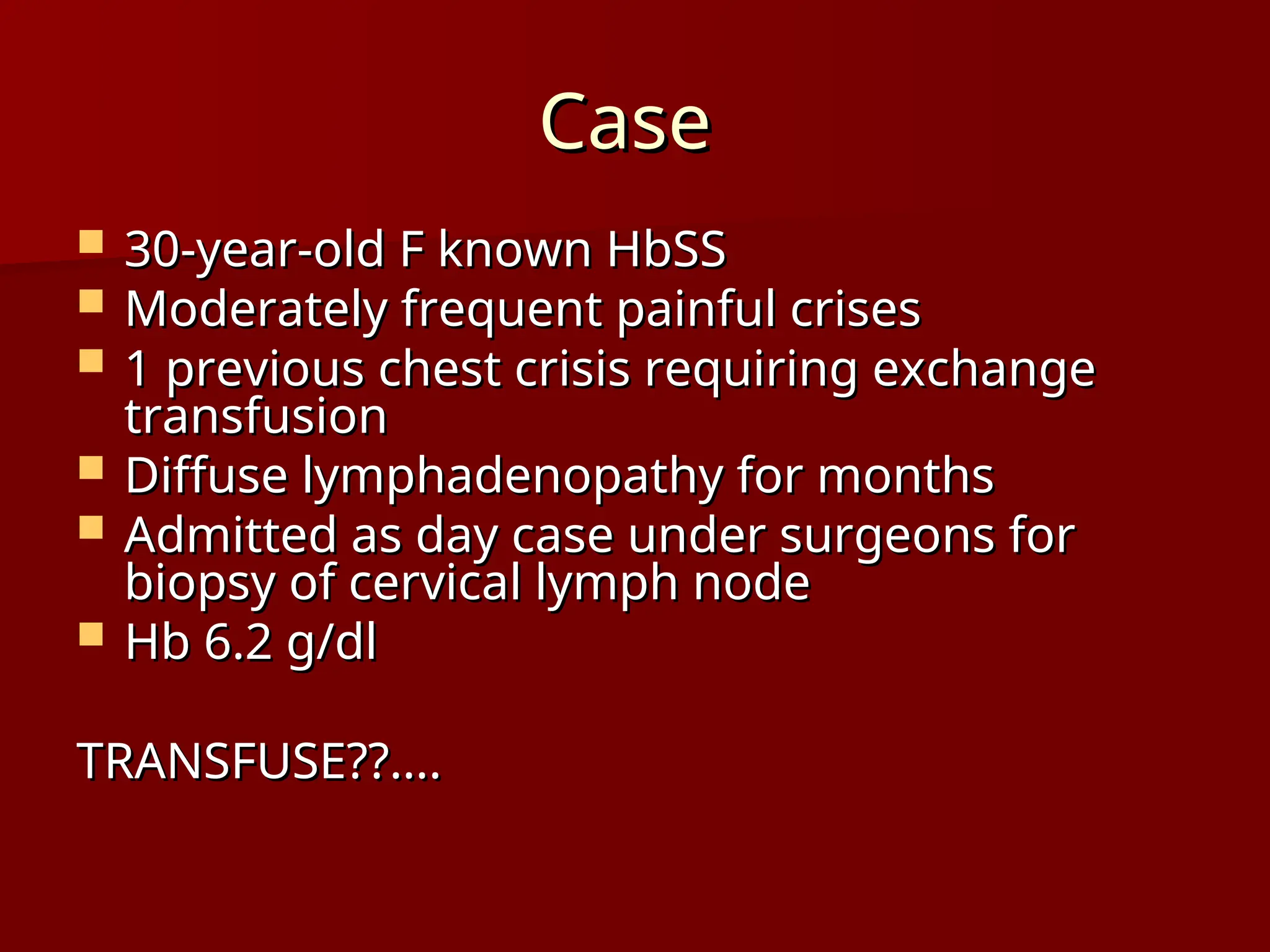
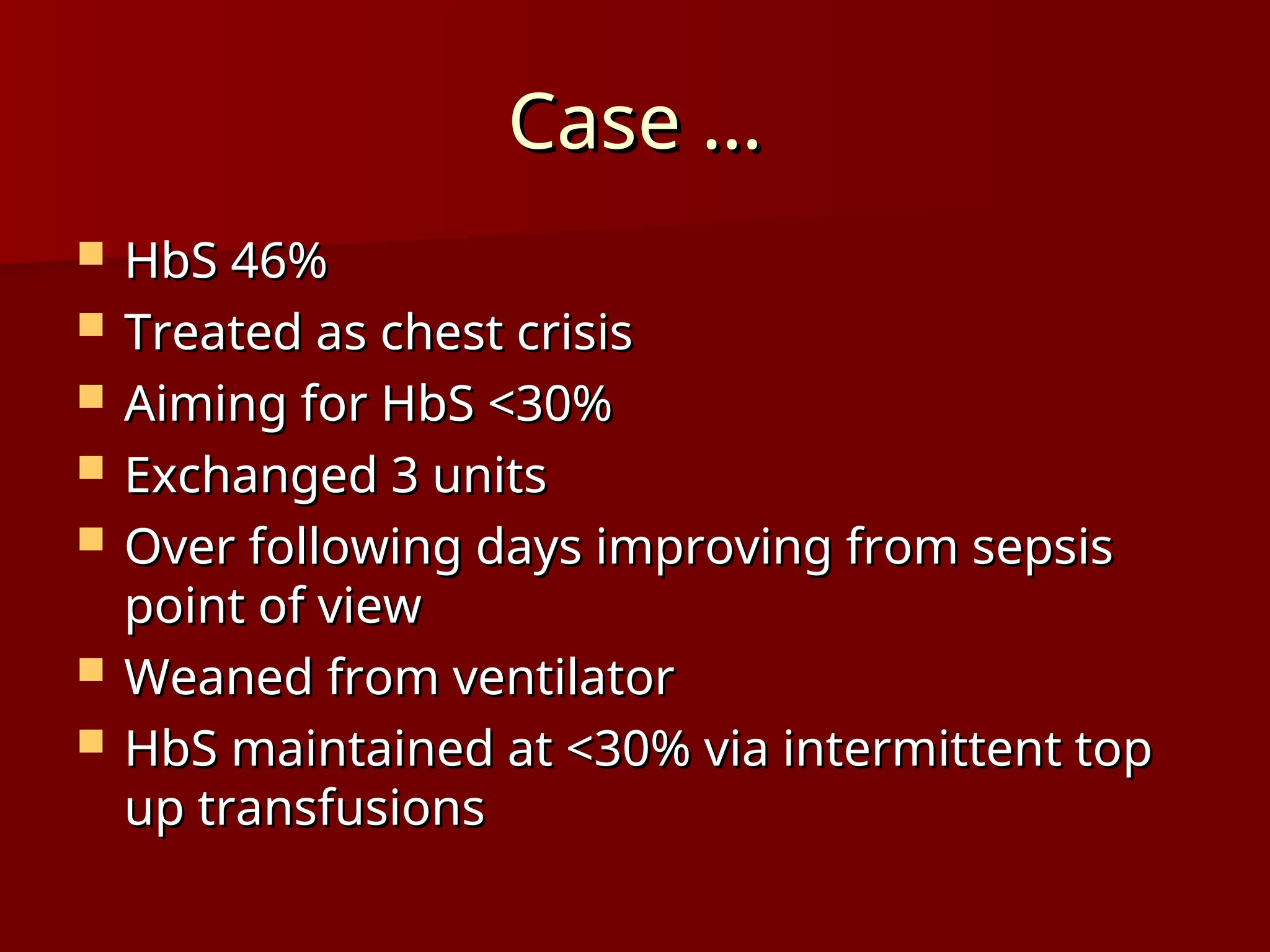
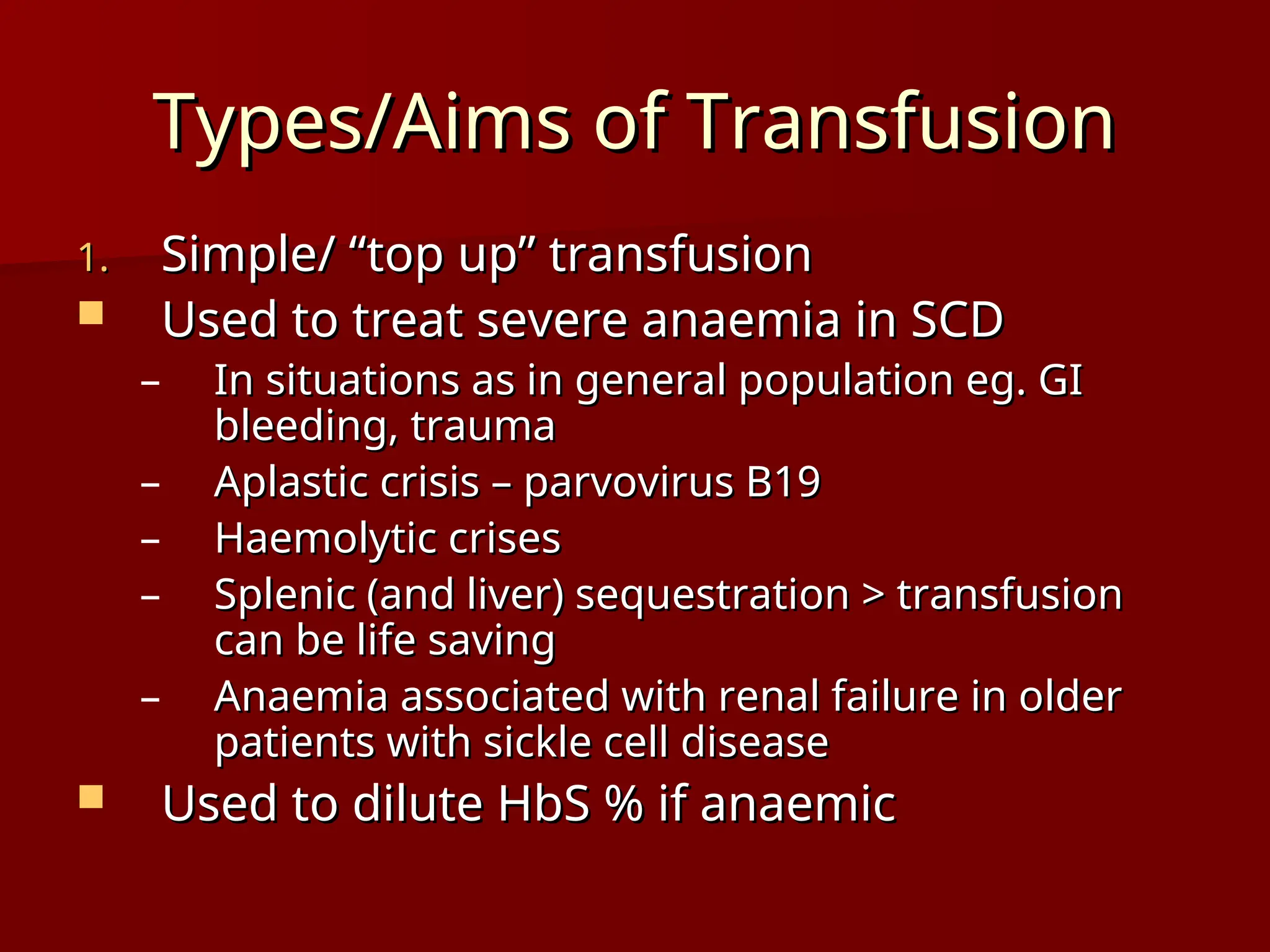
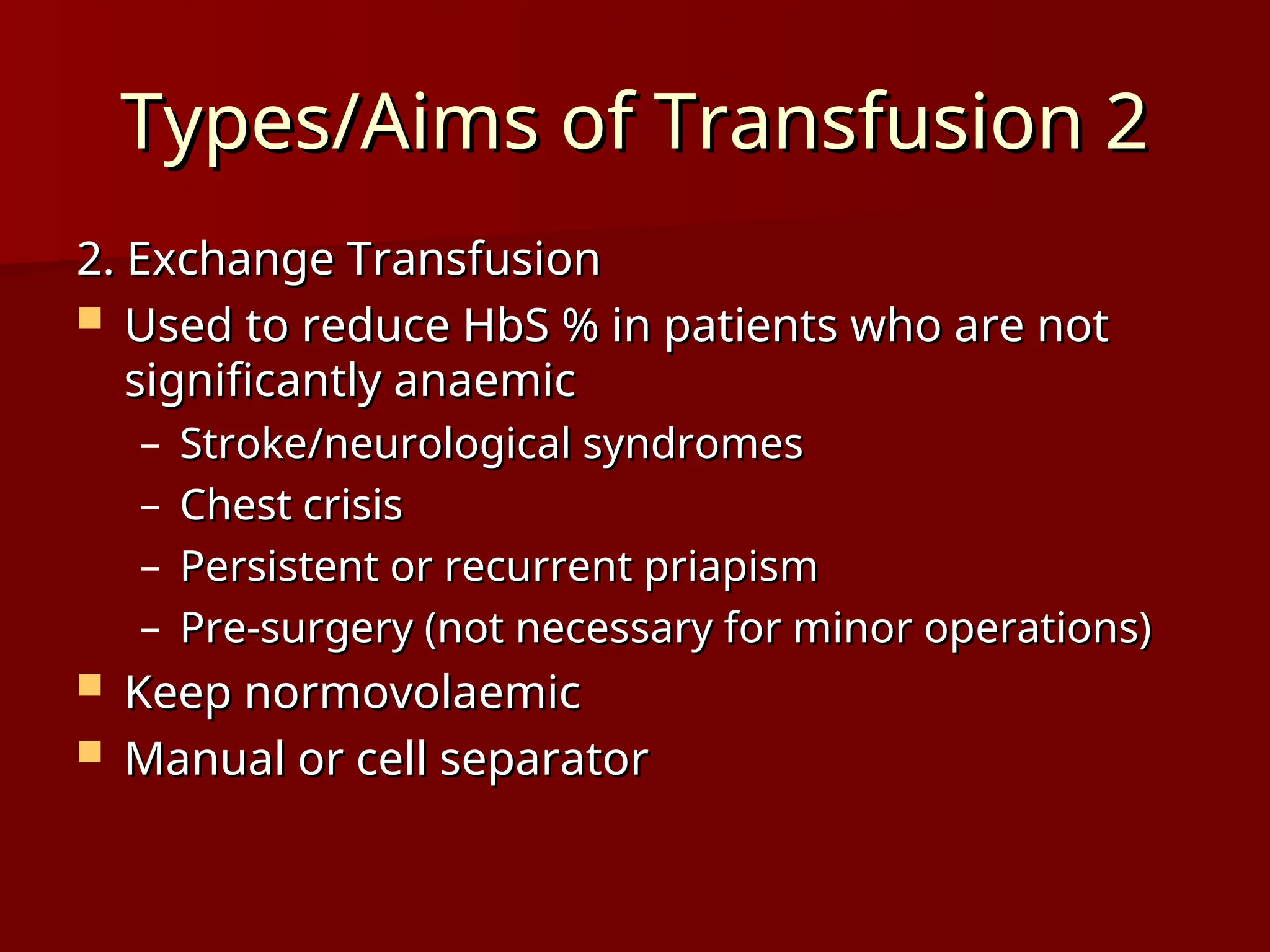
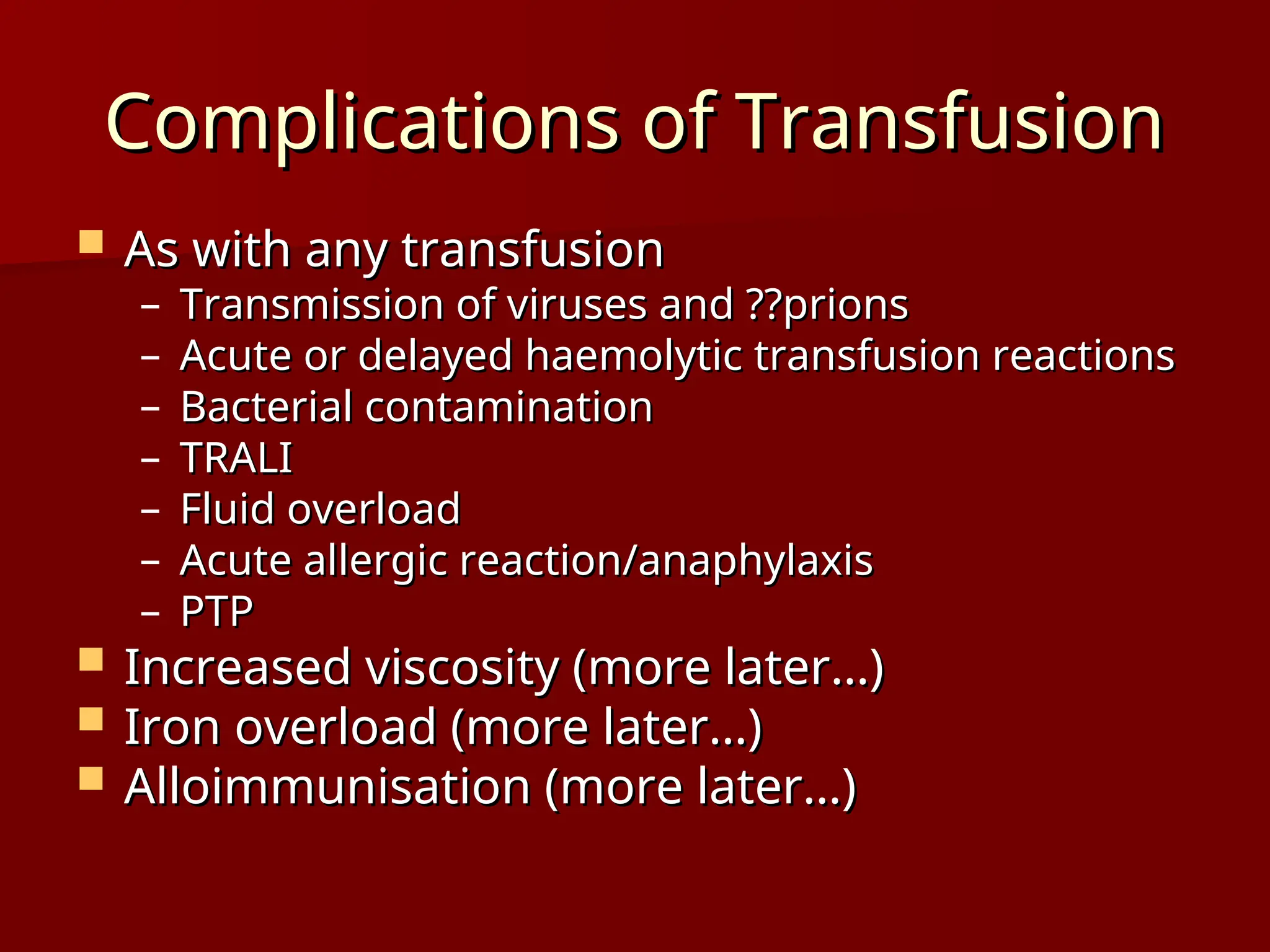
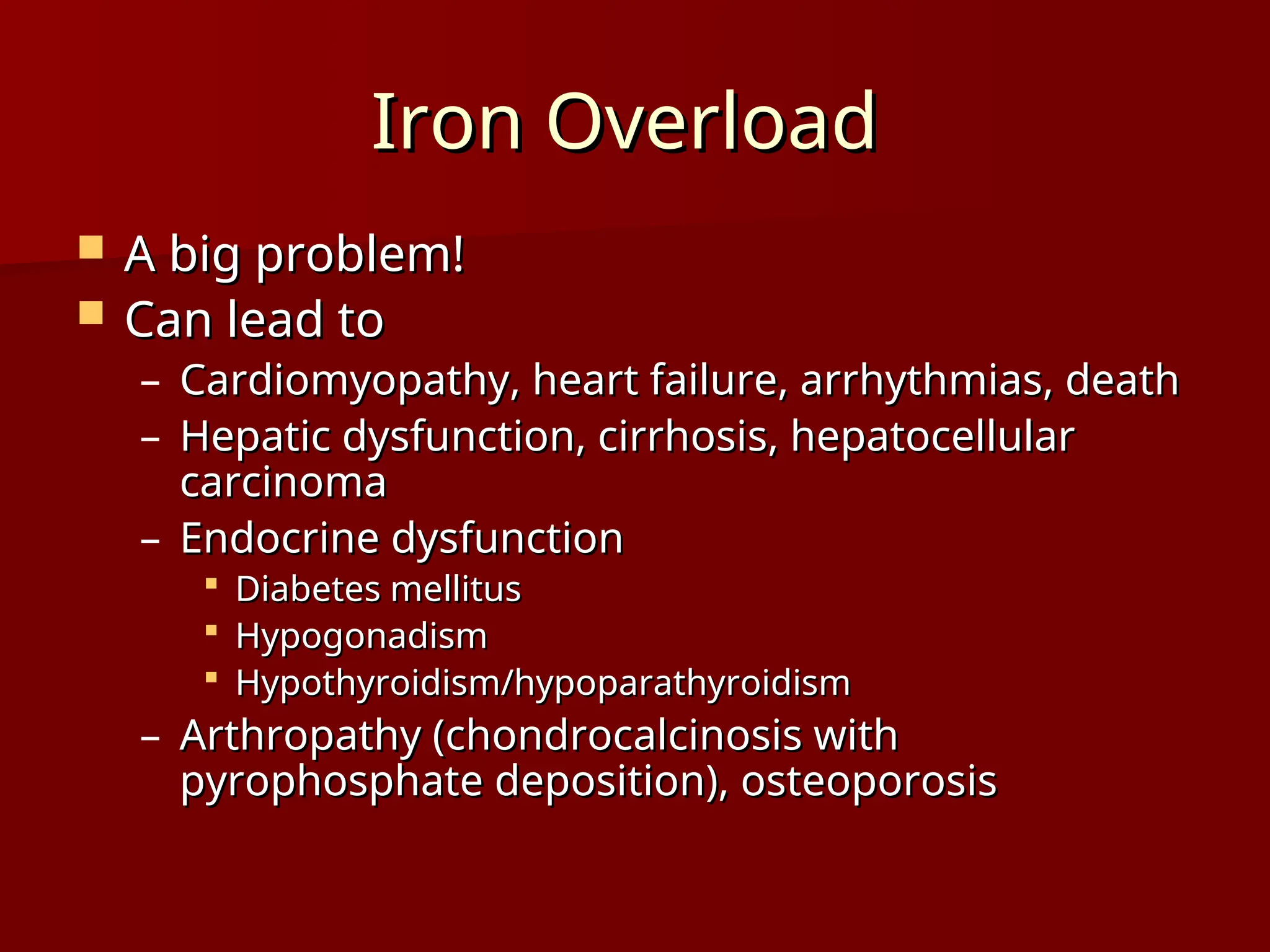
The document discusses the management of blood transfusions in patients with sickle cell disease, including indications for transfusions, the comparison between 'top up' and exchange transfusions, and the complications associated with transfusions. It highlights the importance of monitoring patients for iron overload and alloimmunisation due to frequent transfusions. The document also emphasizes specific precautions to consider when administering transfusions and reviews case studies involving the management of sickle cell crises.