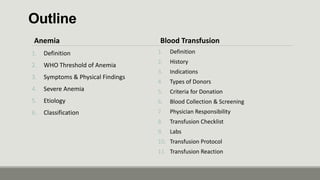
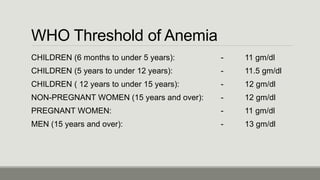
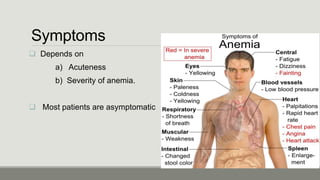
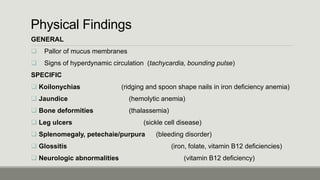
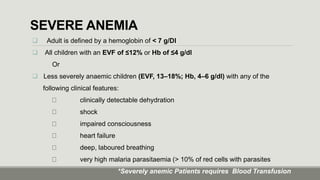
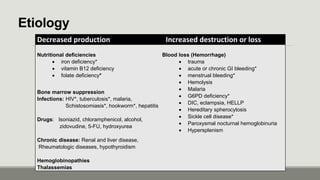
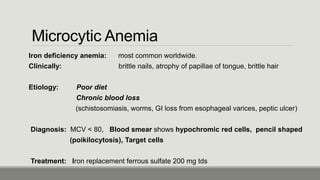
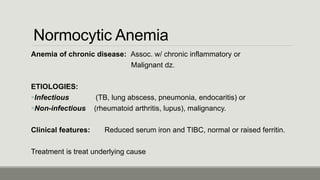
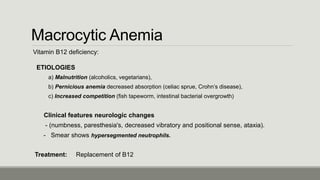
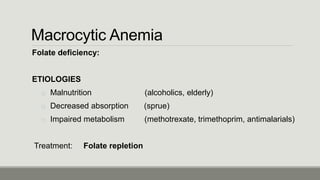
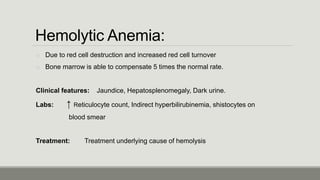
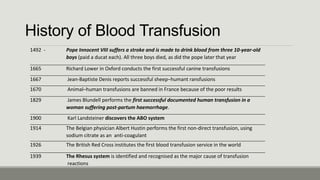
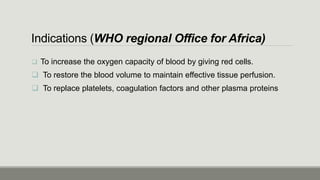
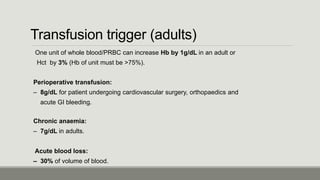
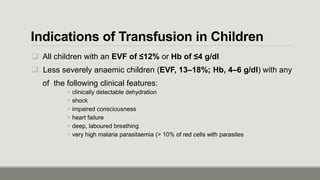
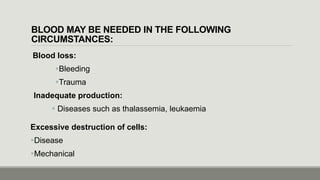
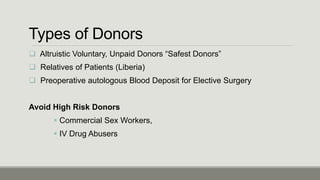
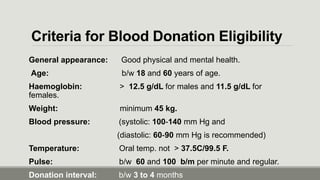
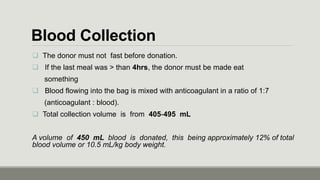
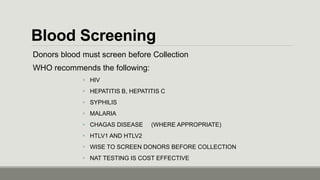
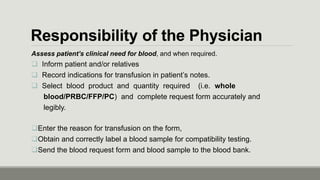
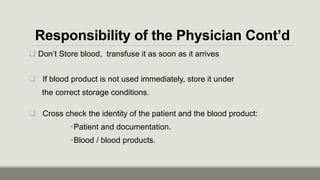
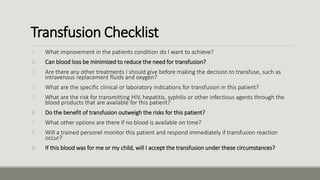
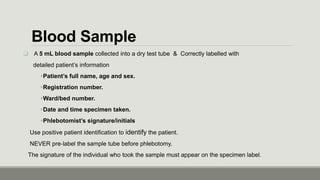
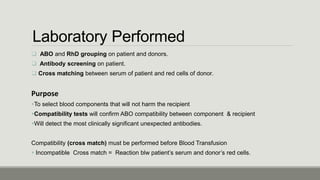
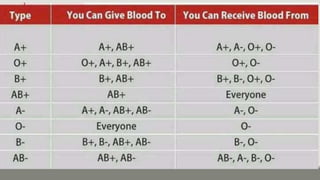
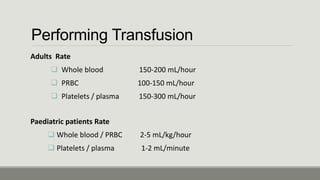
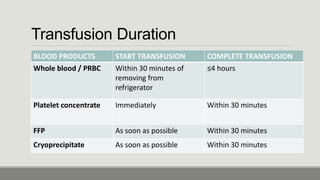
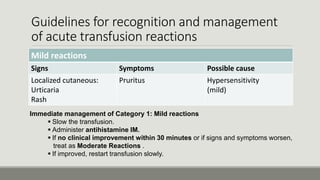
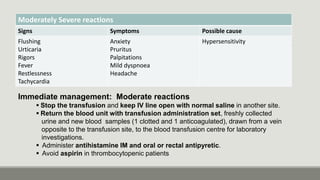
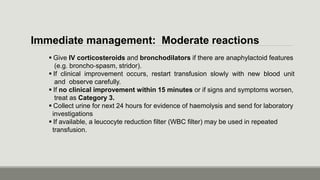
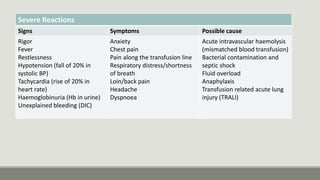
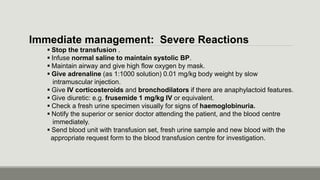
This document provides an overview of anemia, blood transfusion, and transfusion reactions. It defines anemia, describes common causes and classifications. Thresholds for anemia diagnosis are outlined for different populations. Indications for blood transfusion include increasing oxygen capacity and restoring blood volume. The document details donor eligibility, blood collection/screening processes, and guidelines for recognizing and managing transfusion reactions from mild to severe. Physician responsibilities in ordering and administering transfusions are also reviewed.