This document is the title page and table of contents for the book "ABC OF ANTITHROMBOTIC THERAPY" edited by Gregory Y H Lip and Andrew D Blann. It lists the contributors to the book and provides a brief overview of the chapters included, which cover topics such as venous thromboembolism, atrial fibrillation, peripheral vascular disease, anticoagulation monitoring and special circumstances like pregnancy and cancer. The book aims to provide a practical guide to antithrombotic therapy for physicians and other healthcare professionals.










![An overview of antithrombotic therapy
Melagatran
This oral thrombin inhibitor undergoing phase III trials seems Low molecular weight heparin
Unfractionated heparin
to be well tolerated, with few clinically significant bleeding
Enoxaparin sodium (Lovenox) [3.8:1]
problems, in patients with venous thromboembolism. Although
Nadroparin calcium (Fraxiparin) [3.6:1]
considerable pharmacokinetic and animal data exist, solid Dalteparin sodium (Fragmin) [2.7:1]
evidence of its effectiveness compared with warfarin and 0.7
% of composition
heparin in patients at high or low risk is still awaited.
0.6
Heparin 0.5
Heparin is a glycosaminoglycan whose major anticoagulant effect
is accounted for by a pentasaccharide with a high affinity for 0.4
antithrombin III. This binding results in a conformational change 0.3
in antithrombin III so that inactivation of coagulation enzymes
thrombin (IIa), factor IXa, and factor Xa is markedly enhanced. Its 0.2
short half life means it must be given continuously, and its 0.1
extensive first pass metabolism means it must be given
parenterally, preferably by continuous intravenous infusion, and it 0
0 5000 10 000 15 000 20 000
is therefore inappropriate for home use. The effect on the Molecular weight (Da)
intrinsic clotting cascade must be monitored carefully by
Greater antithrombin activity
measuring the activated partial thromboplastin time (APTT),
Greater anti-Xa activity Less anti-Xa activity
generally aiming for a value 1.5 to 2.5 times that of control. Resistant to PF4 Sensitive to PF4
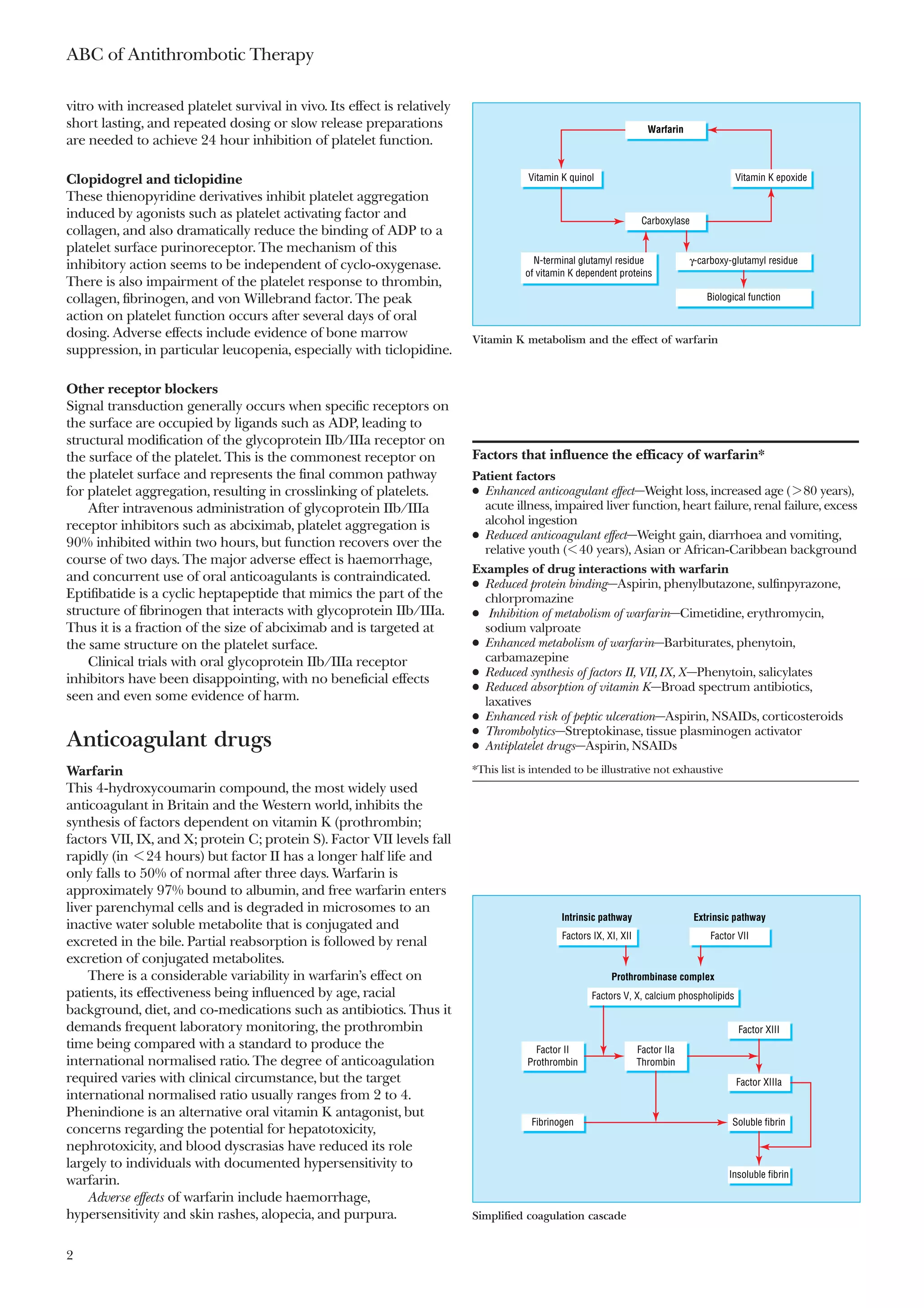
Unfractionated heparin consists of a heterogeneous mixture Little non-specific binding Non-specific binding
of polysaccharides with an average molecular weight of Greater inhibition of thrombin generation Less inhibition of thrombin generation
15 000 Da. Low molecular weight heparins (4000-6000 Da) are
weaker inhibitors of thrombin but inhibit factor Xa to a similar The three low molecular weight heparins that have been evaluated in clinical
trials of acute coronary syndromes are shown with their respective anti-Xa
extent. Different commercial preparations of low molecular and antithrombin activity (PF4=platelet factor 4)
weight heparin vary in the ratio of anti-Xa to antithrombin
activity, although the clinical relevance of this is uncertain. Better
absorption after subcutaneous administration and reduced
protein binding result in greatly improved bioavailability. The
effective half life after subcutaneous injection is four hours,
allowing an injection once daily in most circumstances. These
more predictable pharmacokinetics allow the dose to be
calculated on the basis of the patient’s weight and reduce the Comparison of low molecular weight and unfractionated
requirement for frequent monitoring. In those rare cases where heparins
monitoring is deemed necessary, measurement of plasma levels
of anti-Xa activity is needed. Tests of APTT are unhelpful. Unfractionated Low molecular
Major adverse effects of heparin include haemorrhage, heparin weight heparin
osteoporosis, alopecia, thrombocytopenia, and hypersensitivity. Action Anti-XIIa, XIa, IXa, VIIa, Mostly anti-Xa
antithrombin
At present, the risk of haemorrhage seems to be similar with
Route of Subcutaneous Subcutaneous
low molecular weight and unfractionated heparin. However, the
administration Intravenous
risk of heparin induced thrombocytopenia seems to be less with
Absorption from Slow Improved
the low molecular weight form. subcutaneous route
Protein binding Proteins in plasma and on Reduced
Hirudin and direct thrombin inhibitors endothelium
Hirudin, a 65 amino acid residue anticoagulant peptide with a Bioavailability Subcutaneous—10-30% at > 90%
relative molecular mass of 7000 Da purified from the leech low doses, 90% at higher
Hirudo medicinalis, binds thrombin with high specificity and doses
sensitivity. With a true half life of about an hour and a half life Intravenous—100%
effect on the APTT of two to three hours, it may be seen as an by definition
alternative to heparin in indications such as unstable angina Effective half life Subcutaneous—1.5 hours 4 hours
and in coronary angioplasty. Intravenous—30 min
Many derivatives are available, with hirulog and argatroban Between and within Extensive Minimal
individual variation
among the best developed. However, trials of the former have
Monitoring APTT Not required
been discouraging: no clear benefit over heparin was shown.
(anti-Xa activity)
Conversely, argatroban may have a role in the anticoagulation
Elimination Liver and kidney Kidney
of patients unable to tolerate heparin as a result of heparin
induced thrombocytopenia. Furthermore, in a clinical trial of
patients with heparin induced thrombocytopenia, use of
argatroban was associated with a reduction in levels of plasma
platelet activation markers.
Thrombolytic agents
These agents lyse pre-existing thrombus, either by potentiating
the body’s own fibrinolytic pathways (such as streptokinase) or
3](https://image.slidesharecdn.com/abcofantithrombotictherapy-111115113836-phpapp01/75/Abc-of-antithrombotic-therapy-12-2048.jpg)































































