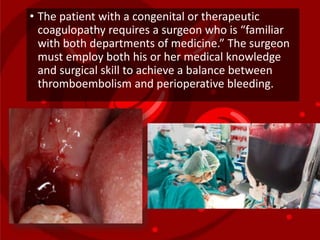
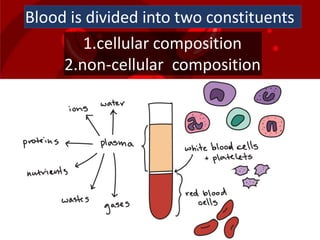
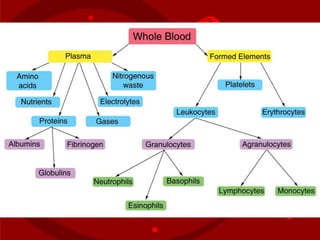
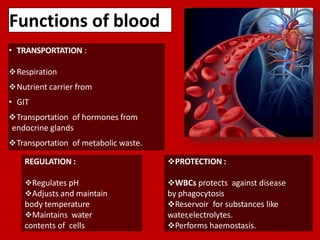
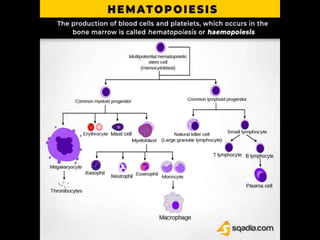
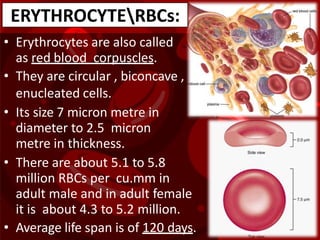
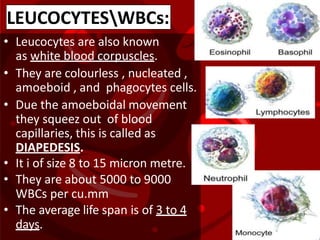
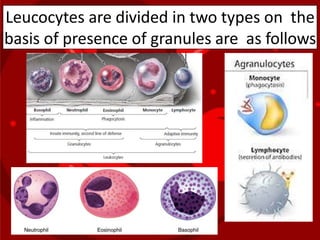
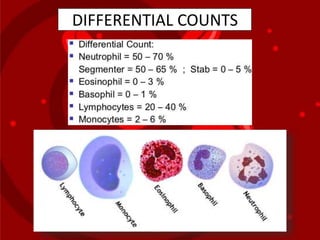
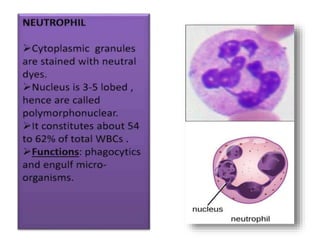
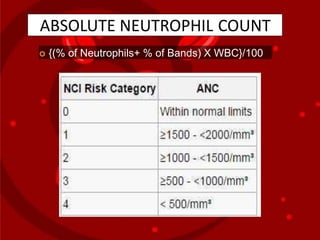
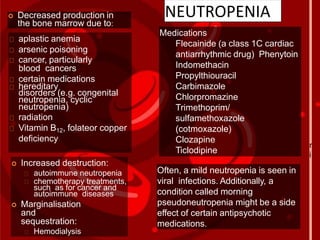
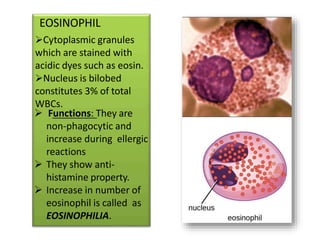
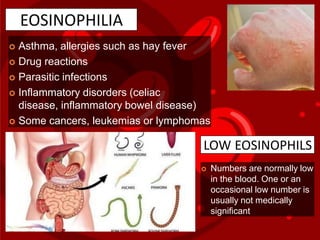
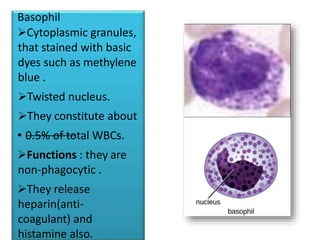
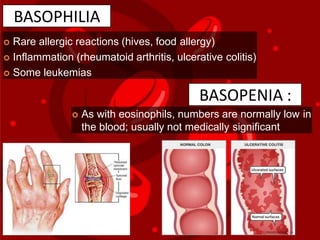
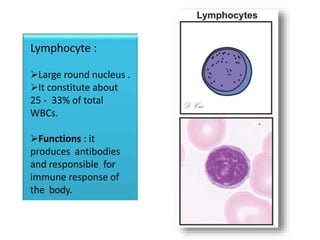
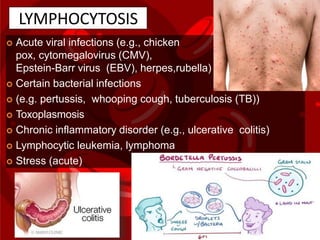
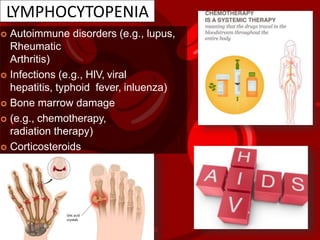
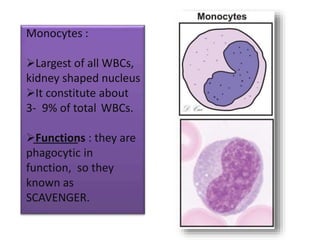
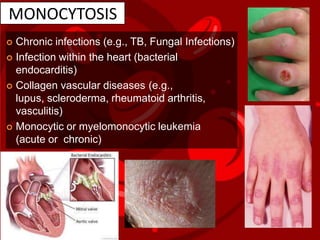
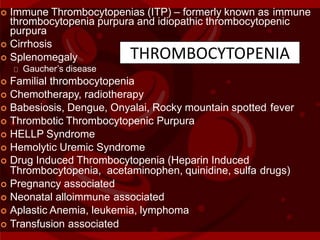
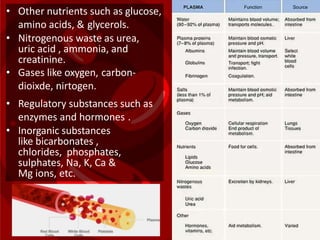
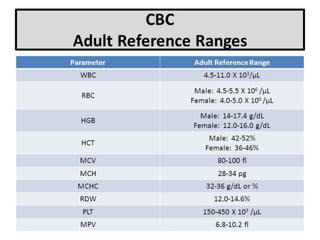
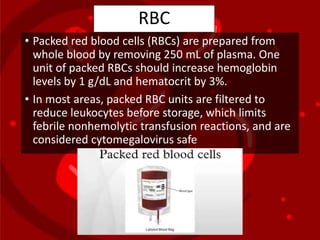
This document provides an overview of blood and its components. It discusses the composition and functions of blood, the cellular components including red blood cells, white blood cells and platelets. It describes complete blood count tests and normal ranges. Conditions that cause increases or decreases in various blood cell counts are outlined. The document emphasizes the importance of understanding blood and hemostasis as an oral surgeon dealing with medically compromised patients.



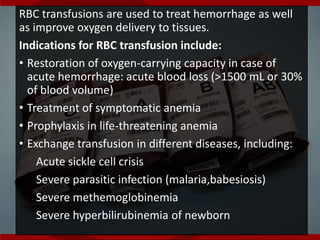
![• Recommended dosage and administration include:
• One unit of RBC increases the hemoglobin level of an
average-sized adult by w1 g/Dl (or increases hematocrit
w3%)
• The ABO group of RBC products must be compatible
with the ABO group of the recipient
• Ideally, the RBC product must be serologically
compatible with the recipient
• Rate of transfusion
• Transfuse slowly for the first 15 minutes
• Complete transfusion within 4 hours (per US Food and
Drug Administration [FDA])](https://image.slidesharecdn.com/1finalpresentationblood-191207143958/85/Blood-52-320.jpg)