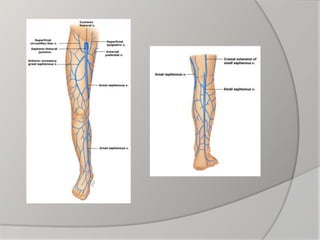
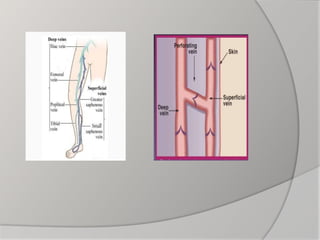
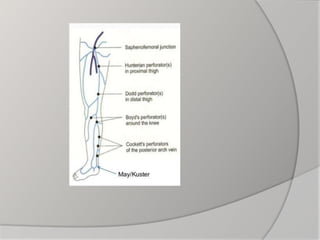
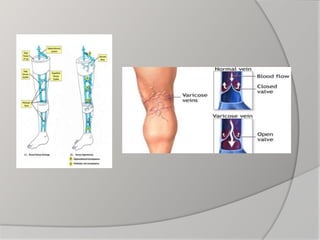
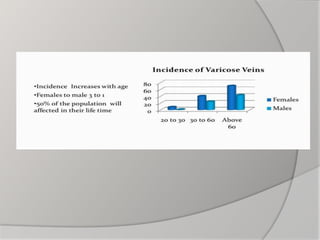
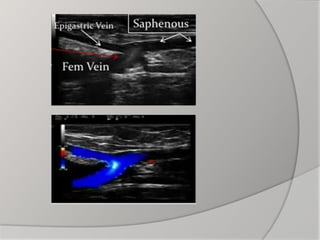
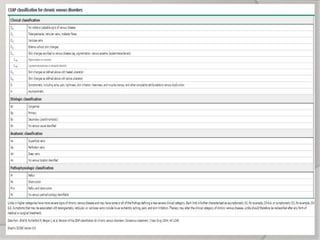
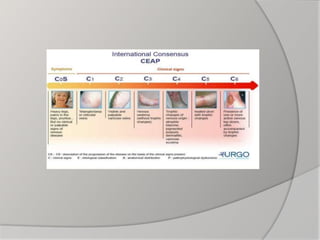
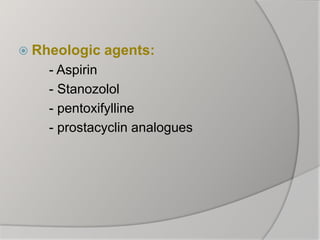
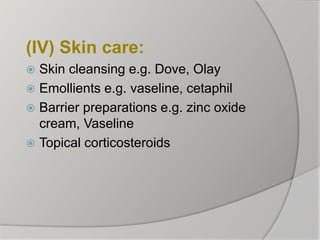
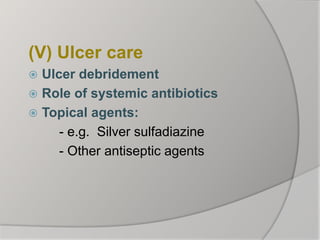
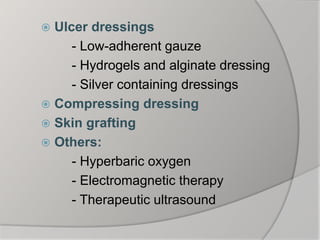
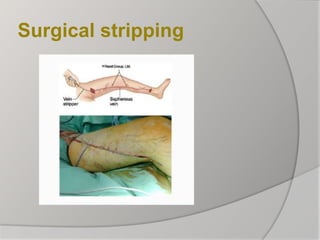
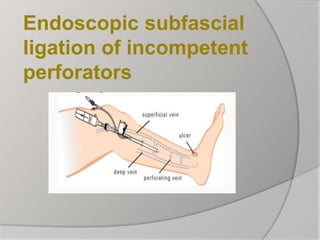
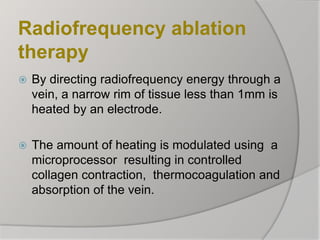
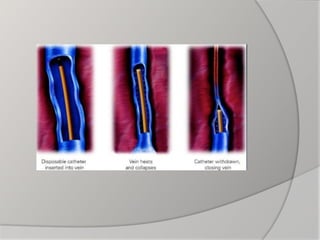
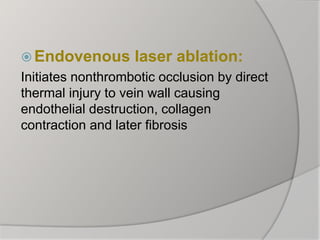
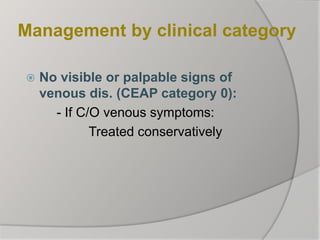
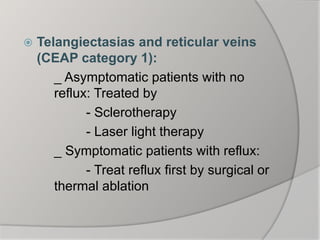
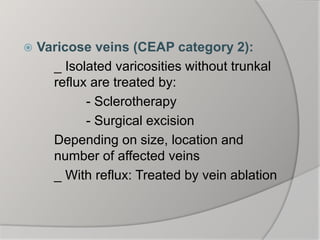
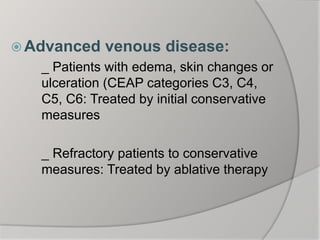
This document discusses varicose veins (VV), including their definition, anatomy, pathophysiology, etiology, clinical presentation, investigations, treatment options, and management approach. VV are dilated, tortuous superficial veins in the lower limbs. Treatment involves initial conservative measures for 3 months, including compression therapy and pharmacologic agents for symptomatic patients or those with reflux. Refractory patients may undergo ablative therapies like sclerotherapy, radiofrequency ablation, or laser ablation to treat refluxing veins. The goals of treatment are improved symptoms and appearance.