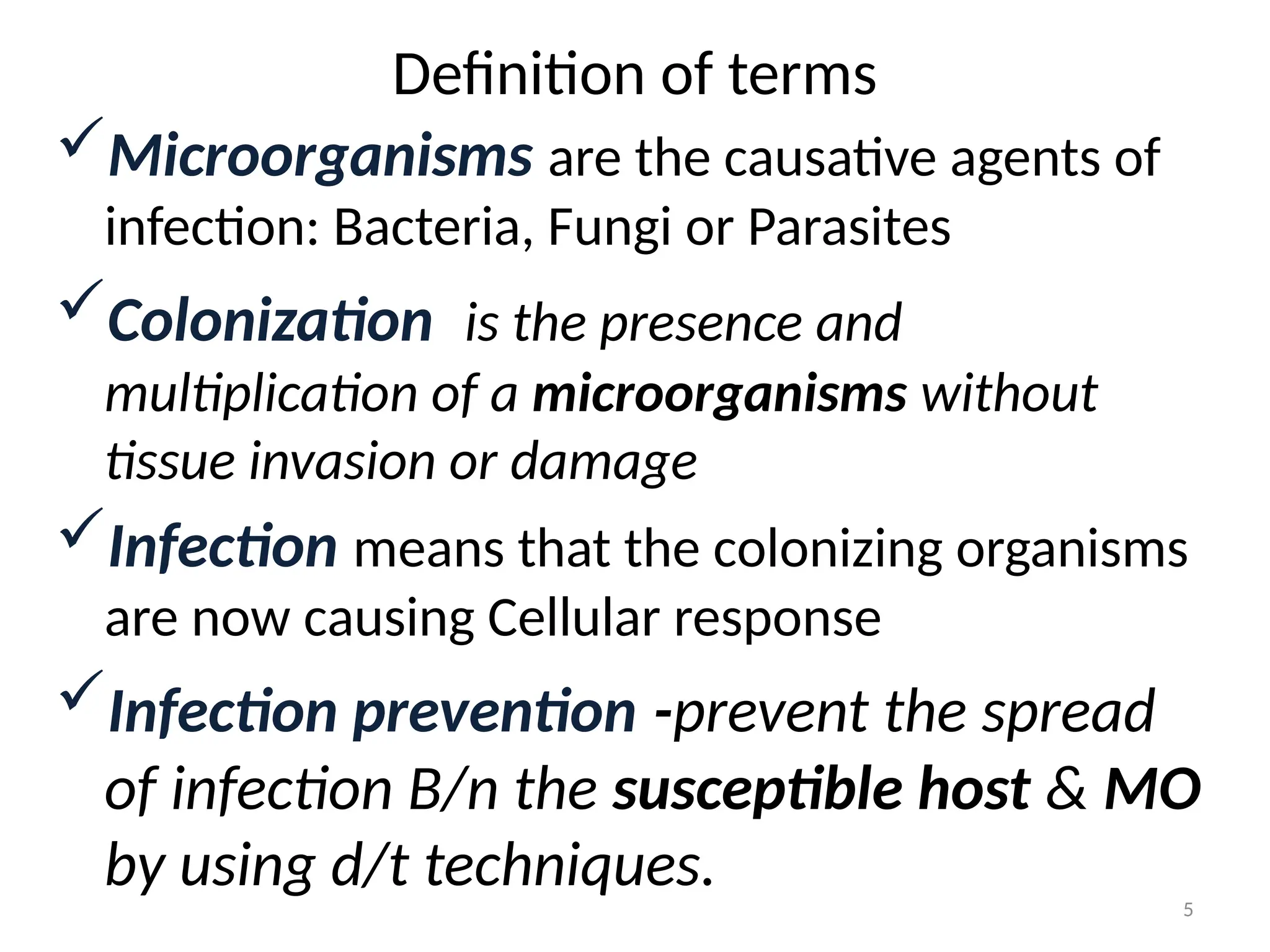
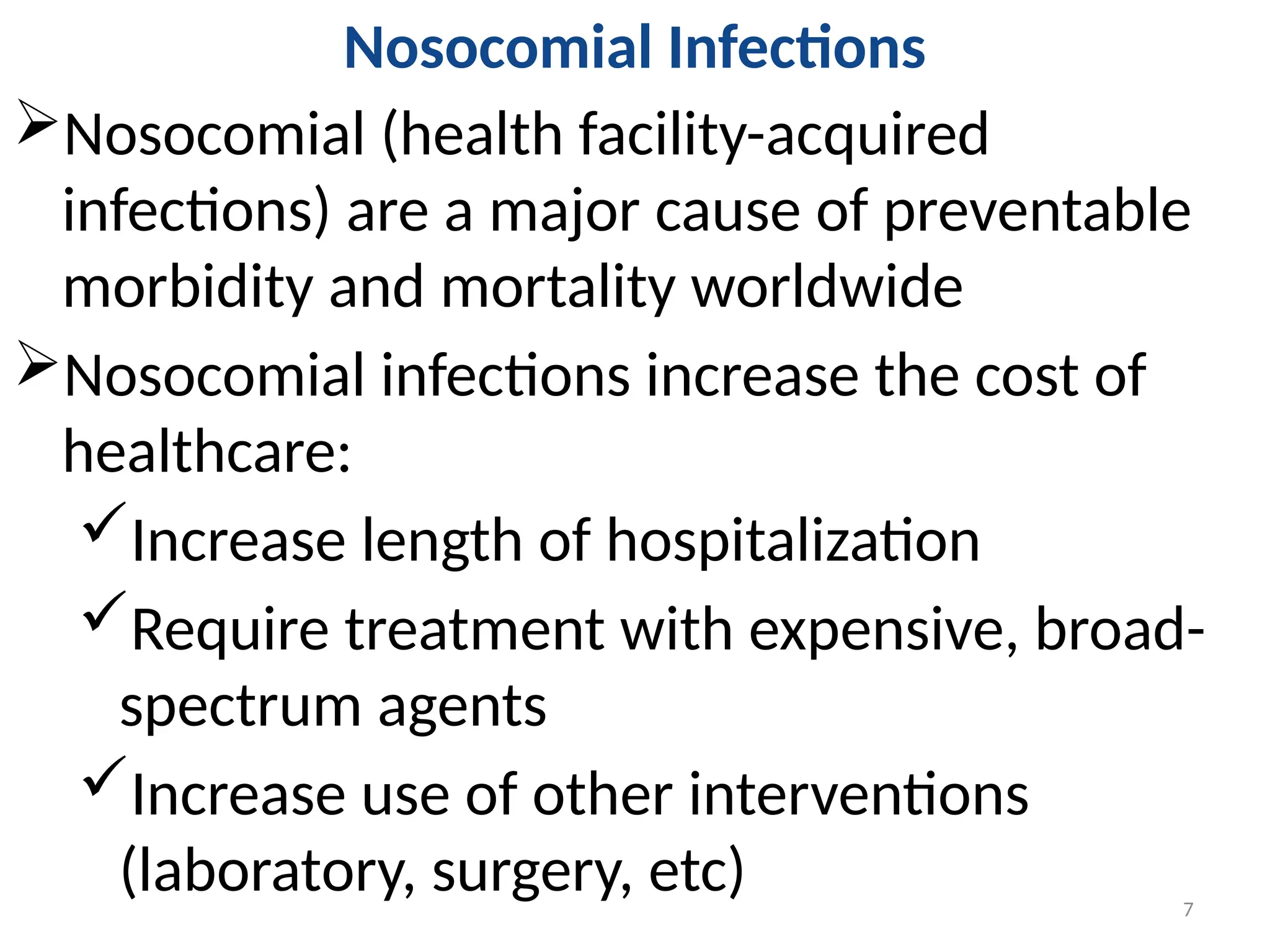
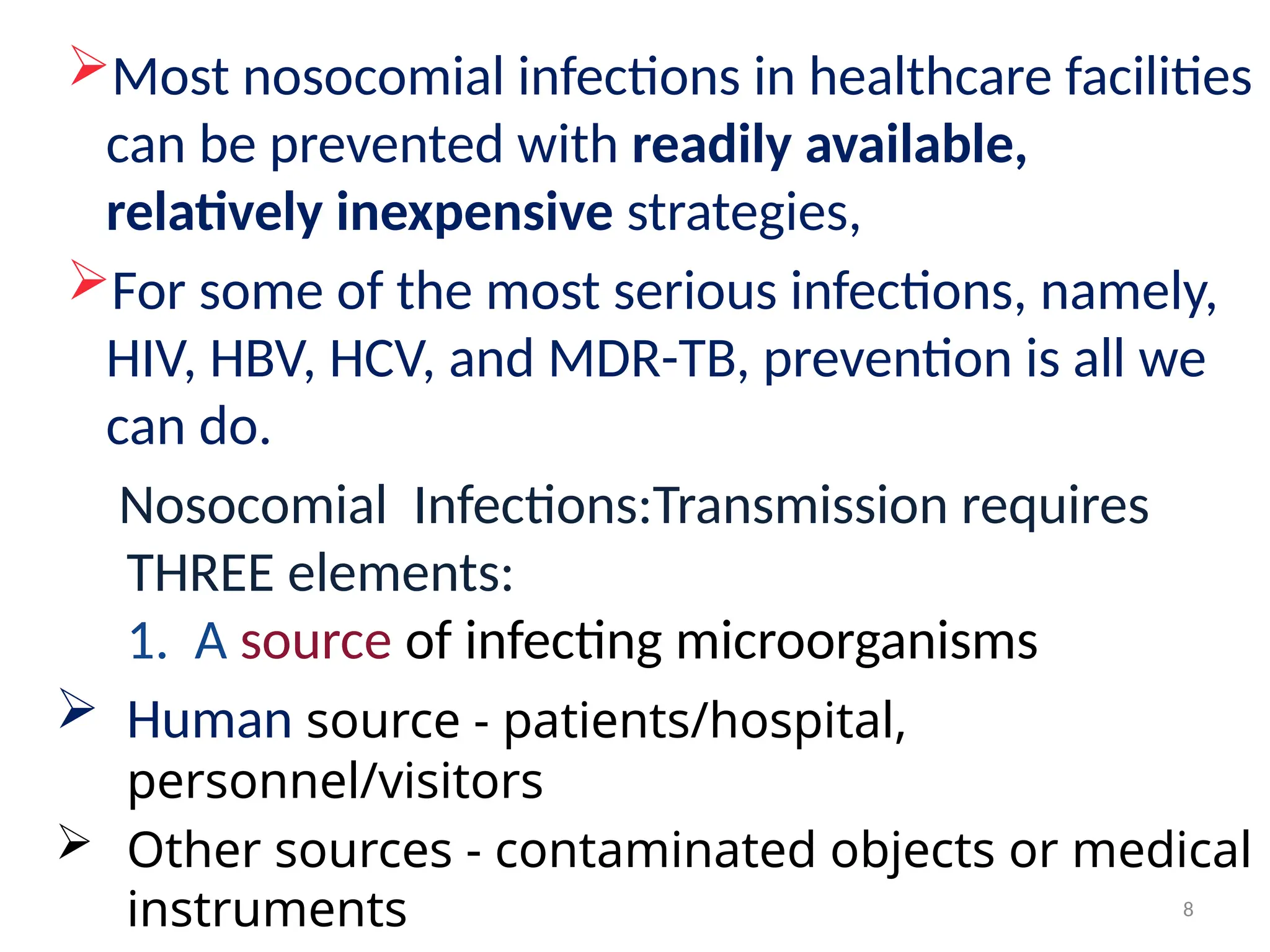
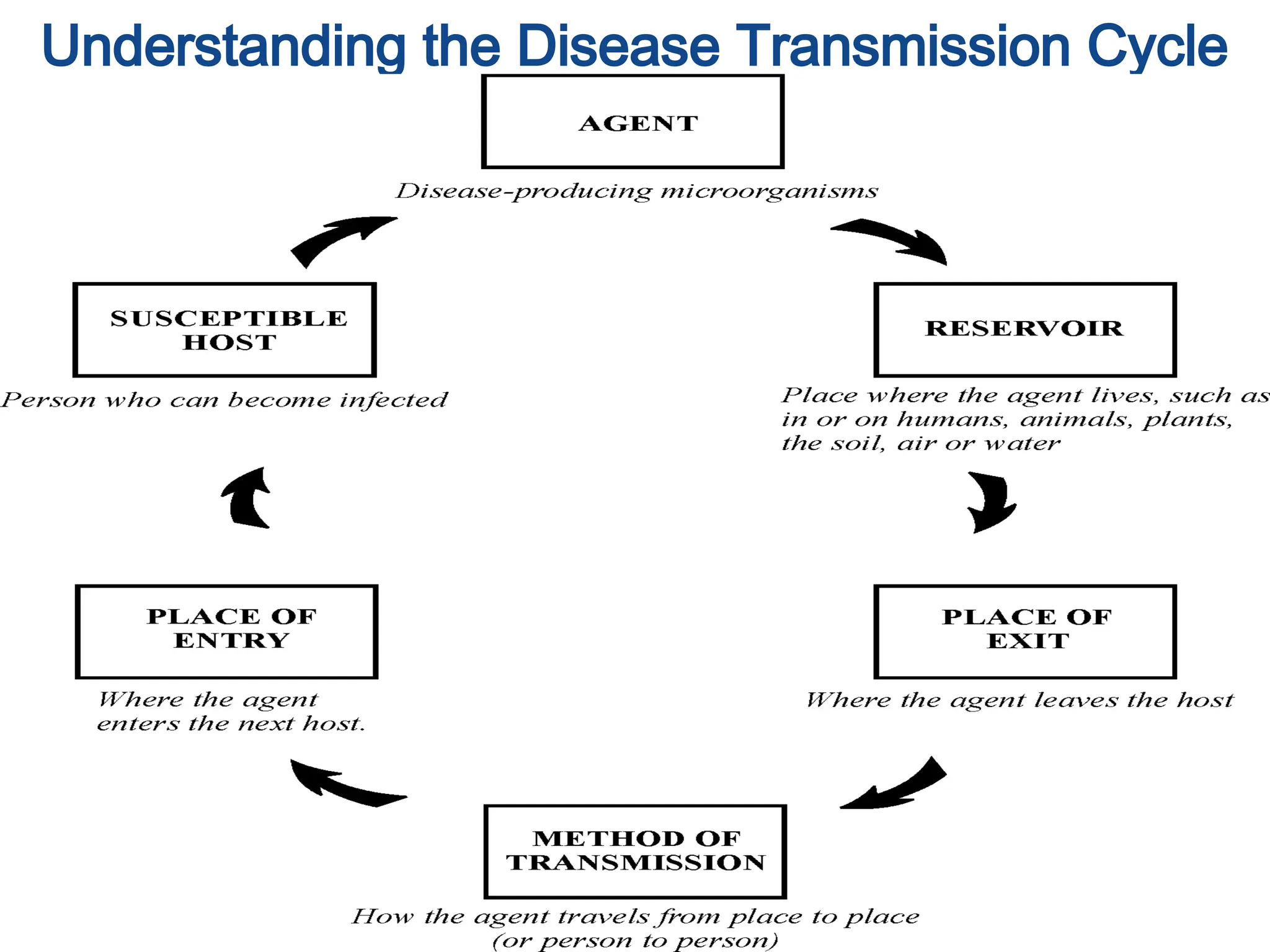
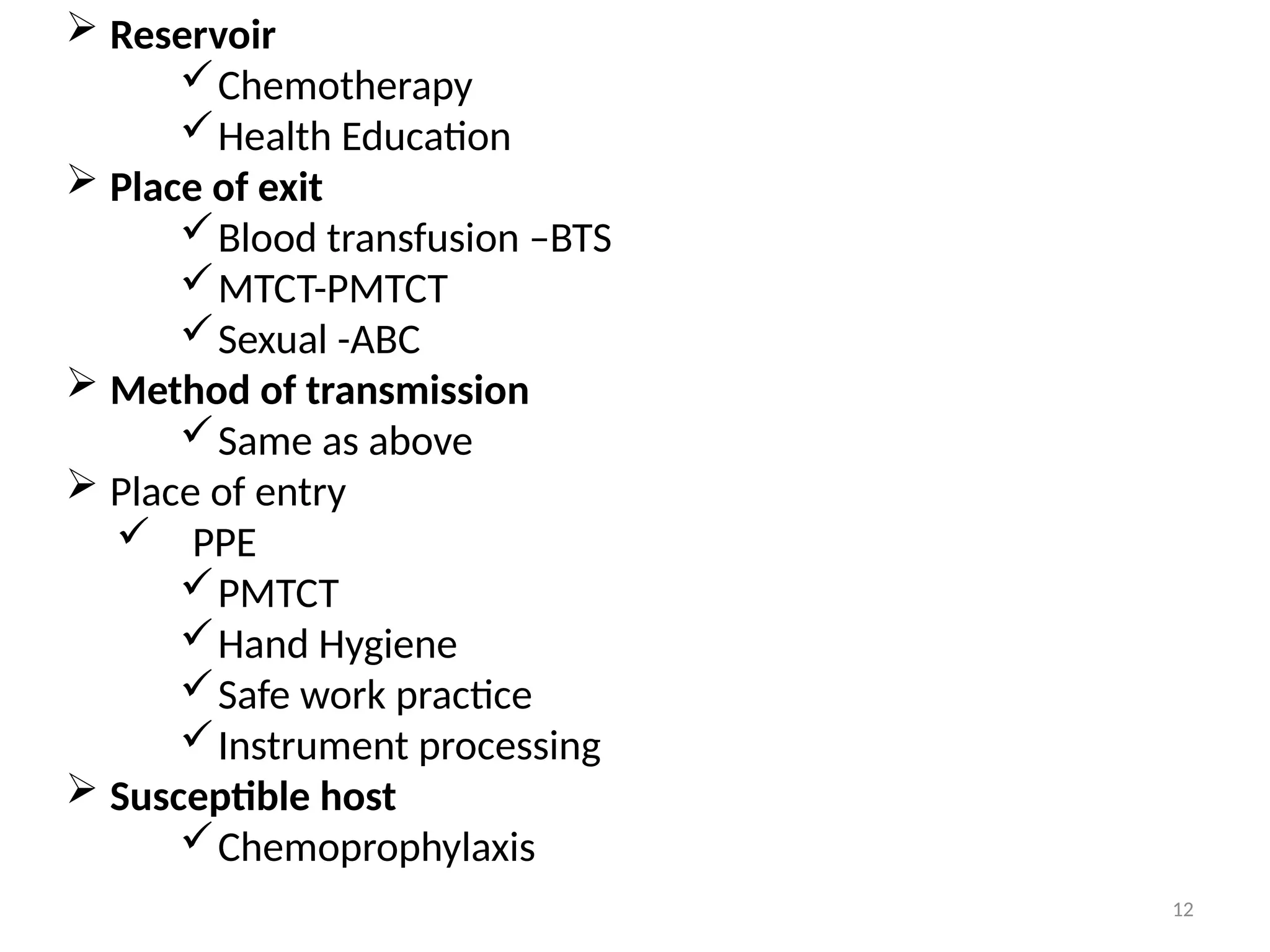
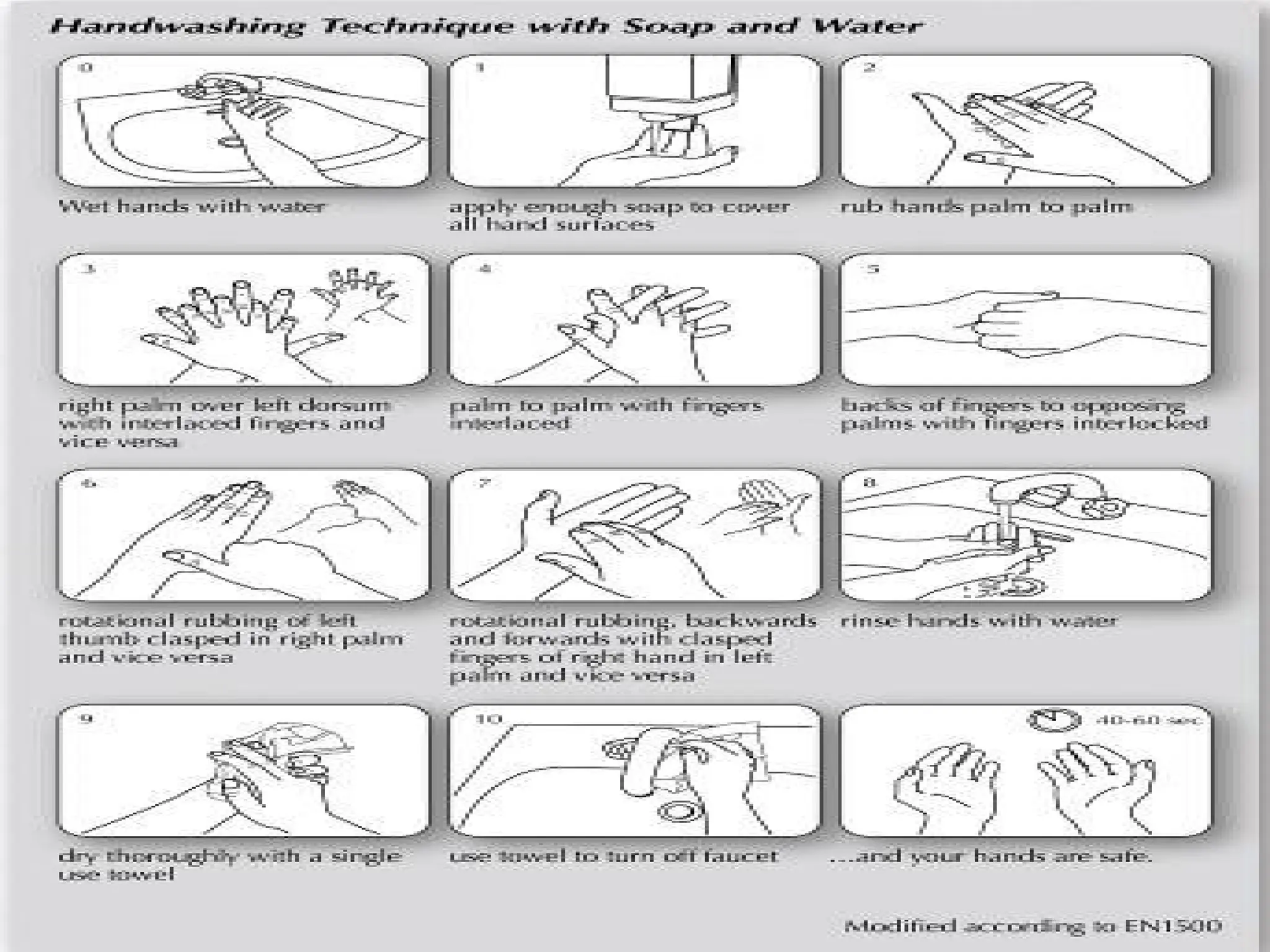
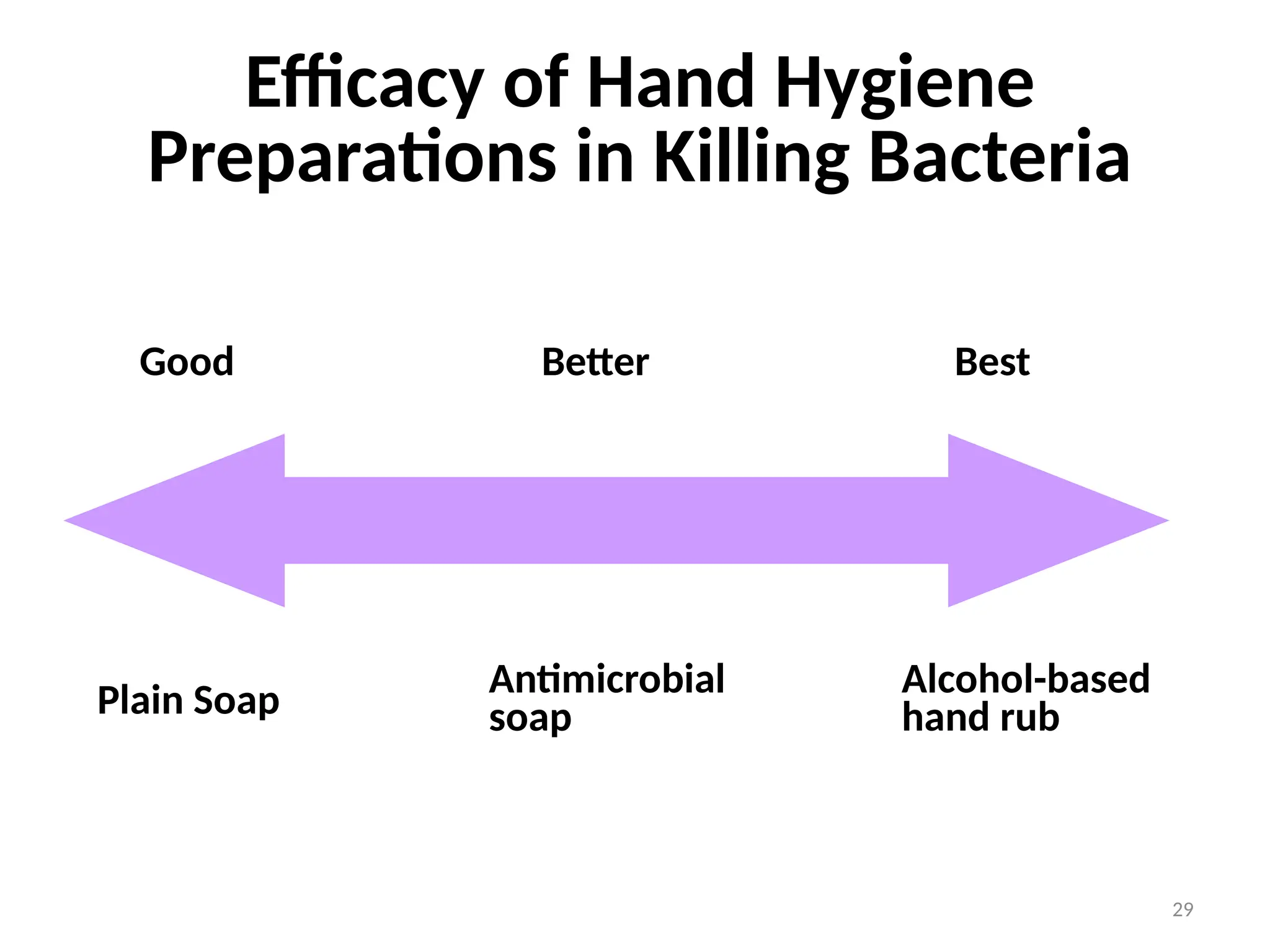
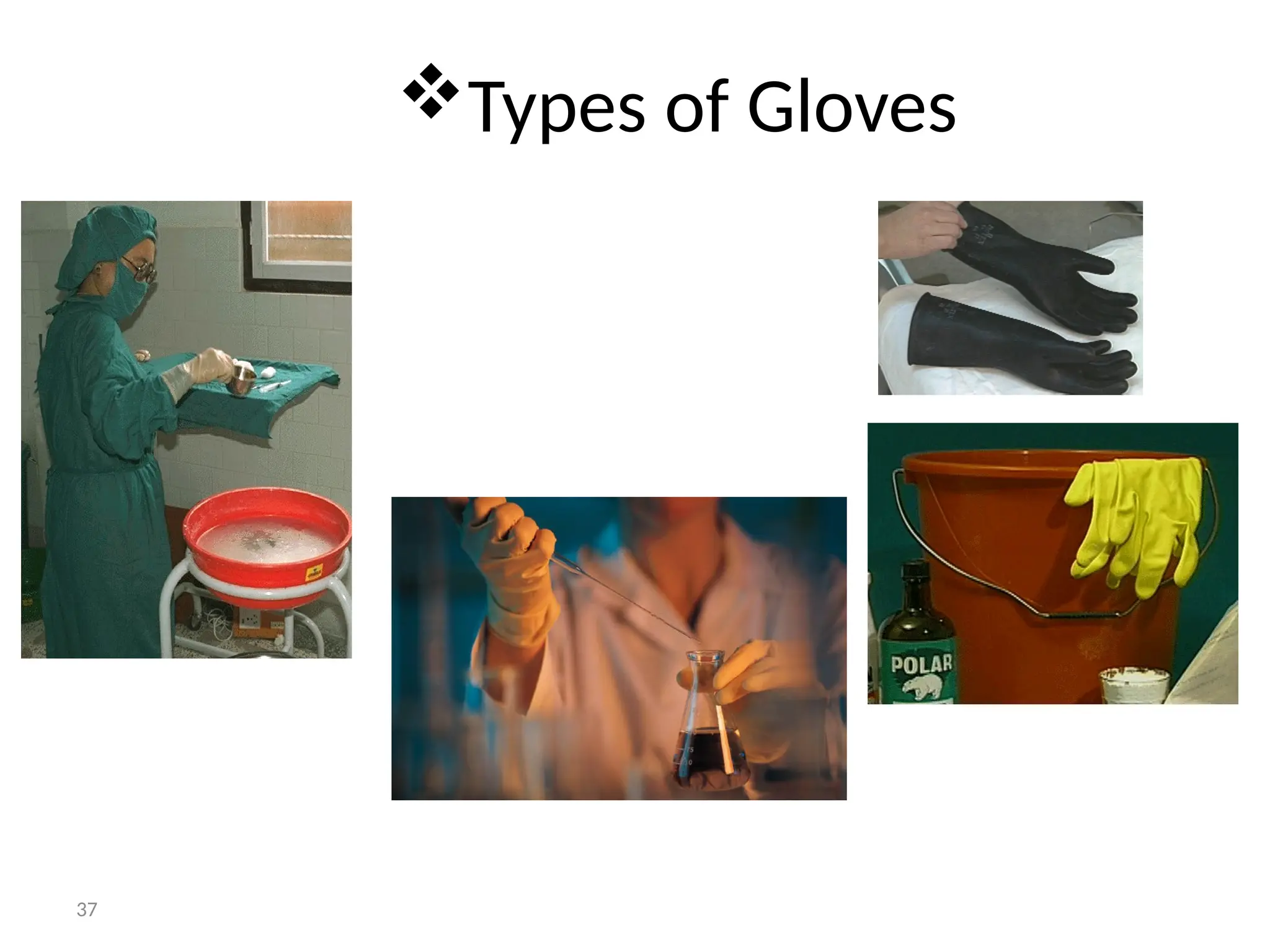
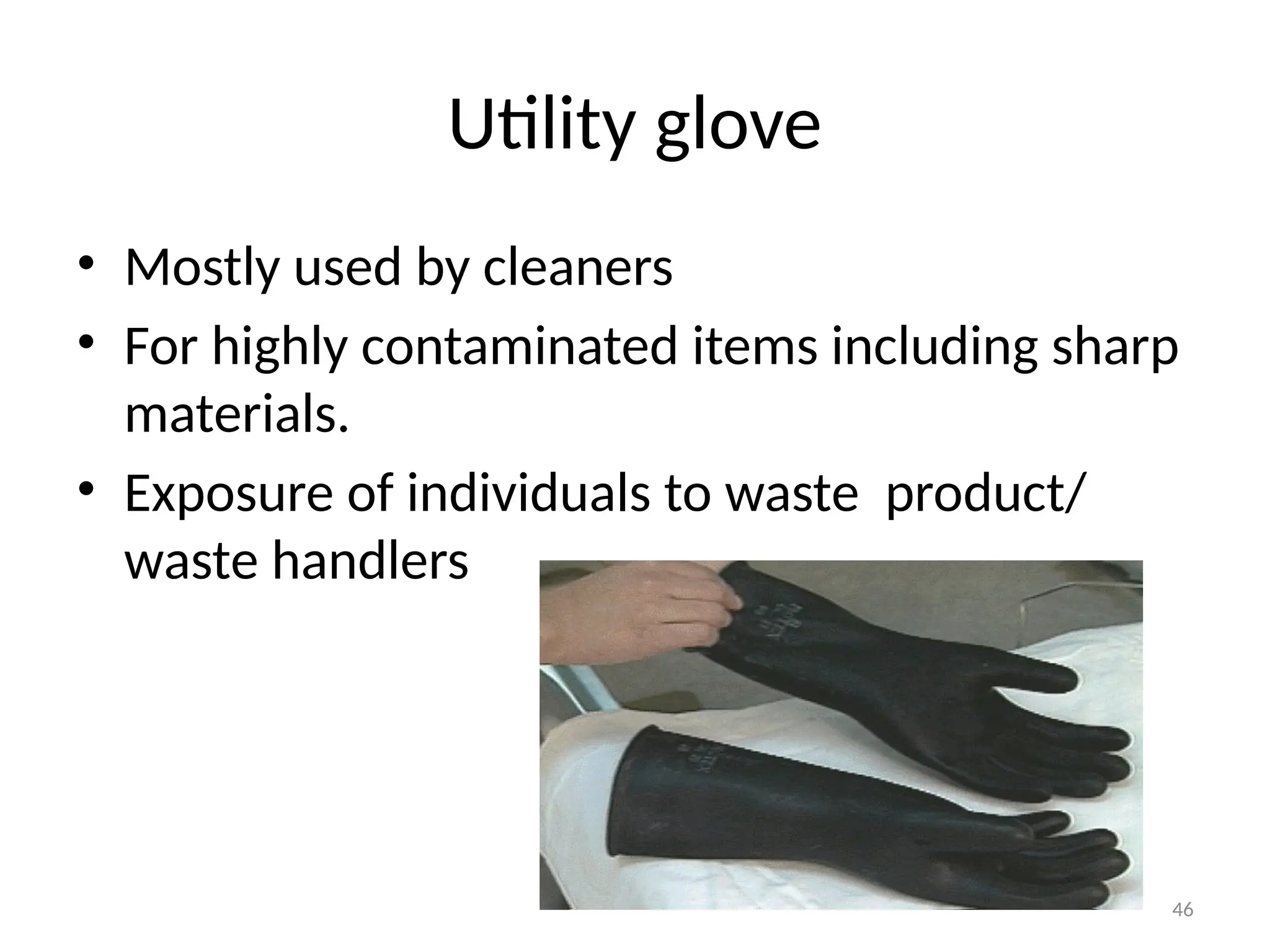
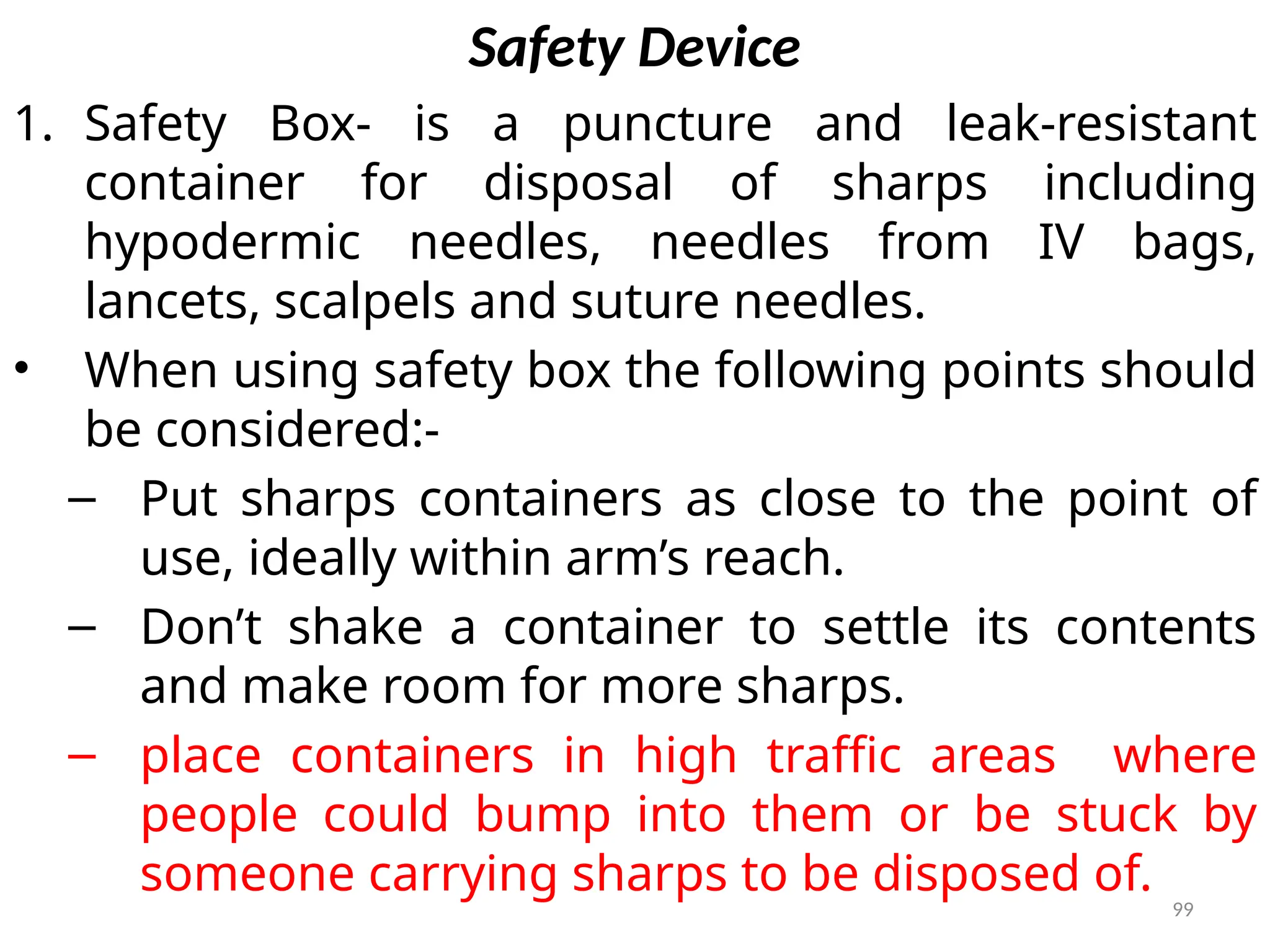
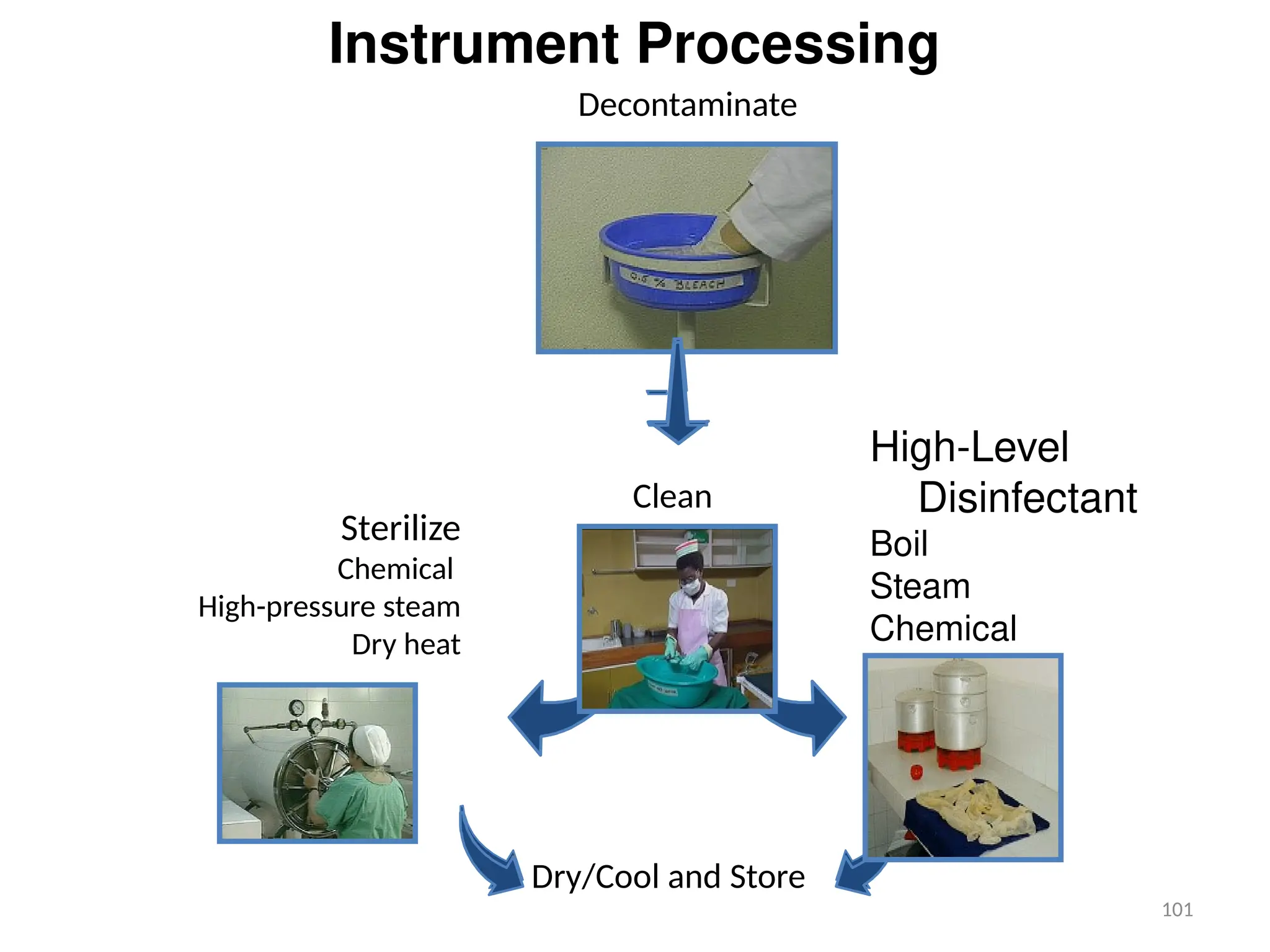
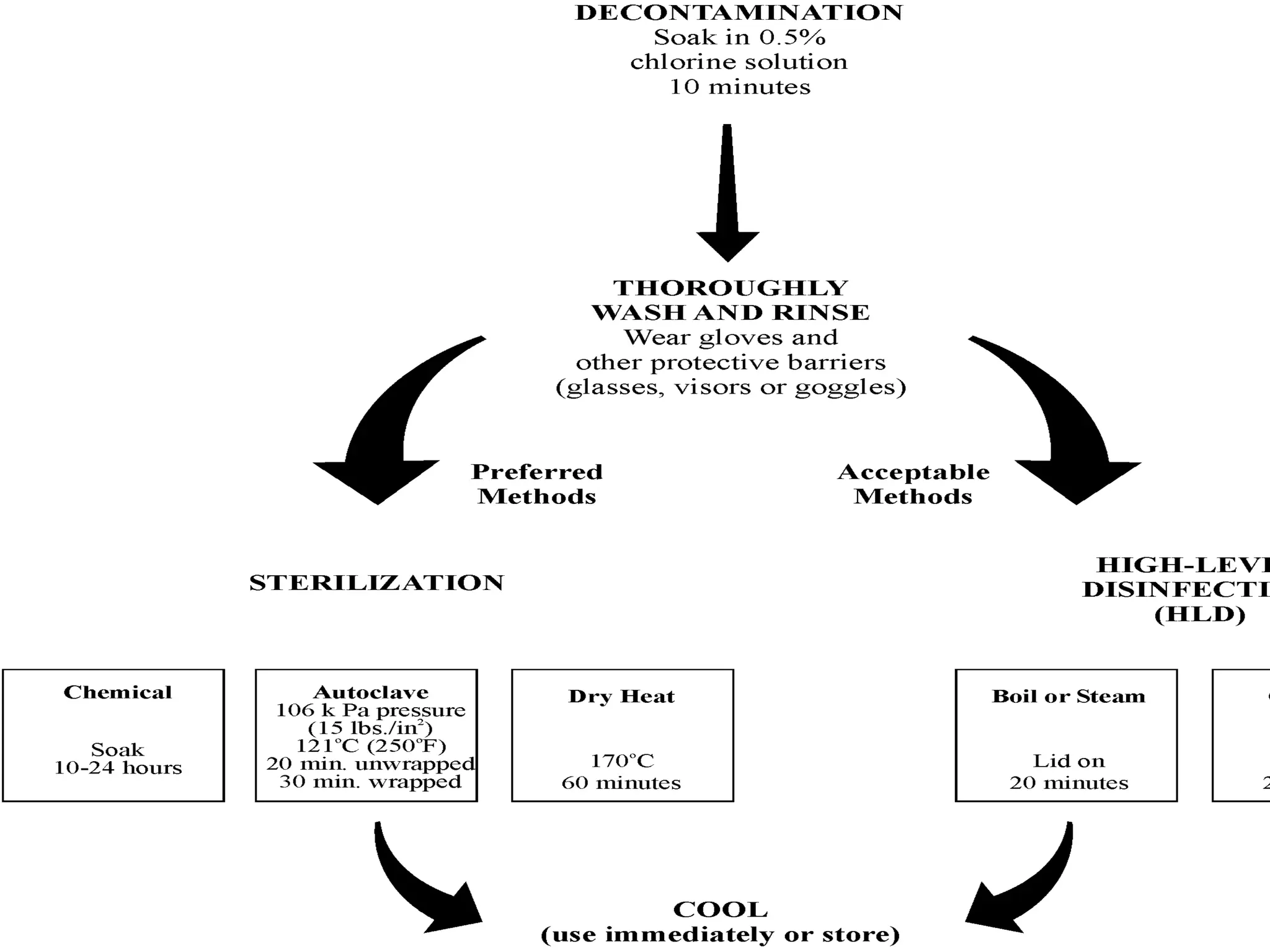
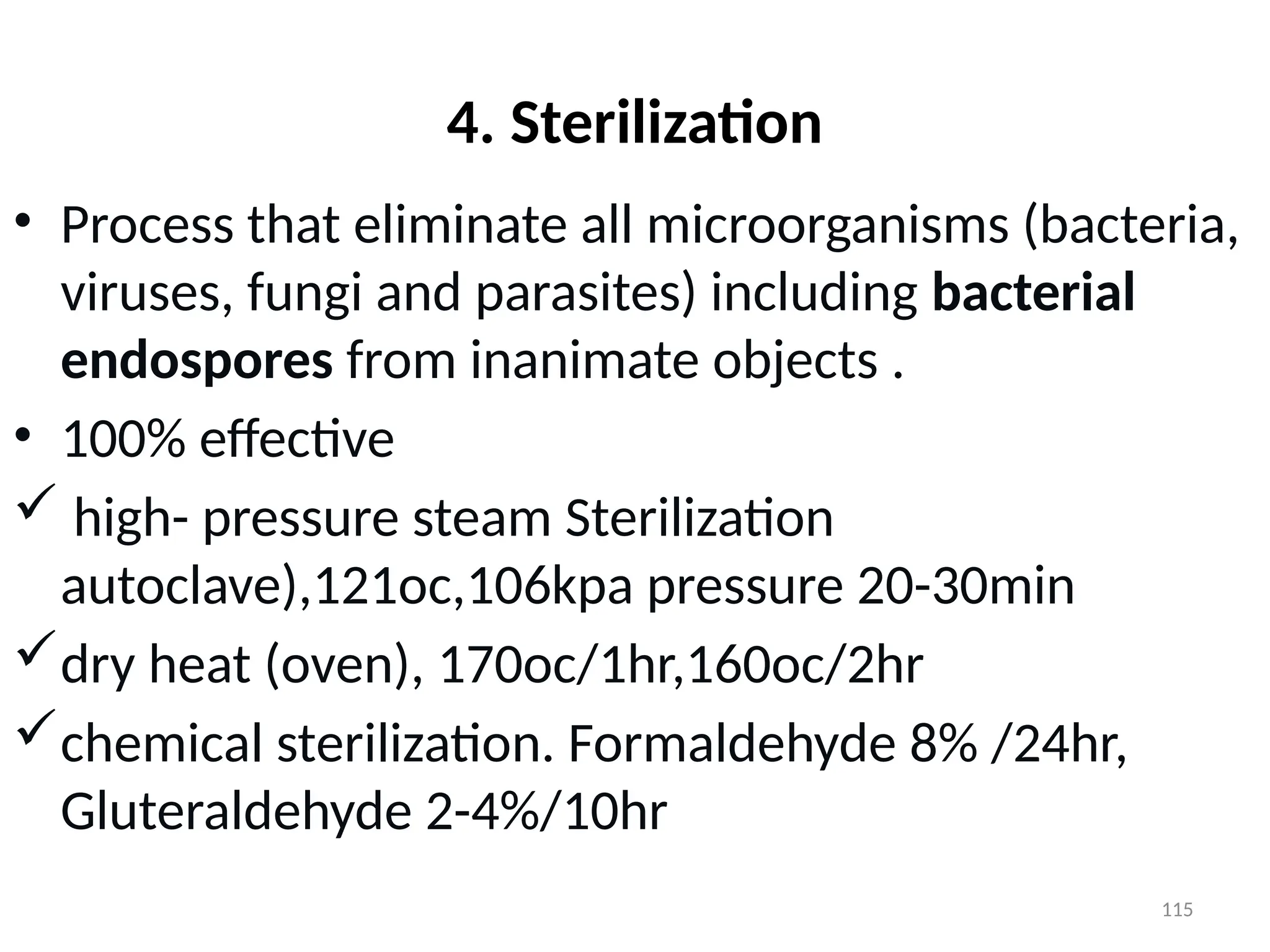
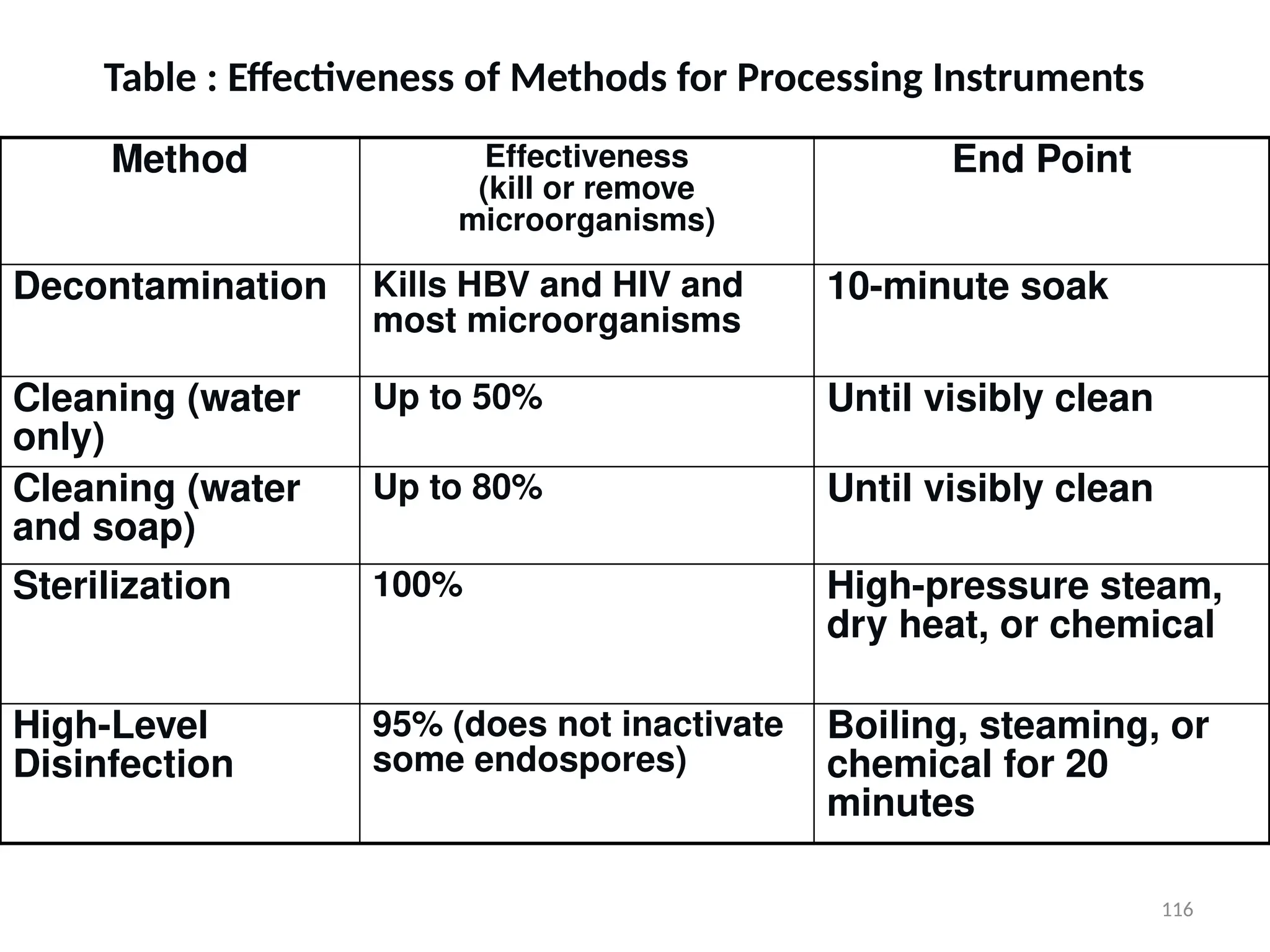
This document provides a comprehensive overview of infection prevention and patient safety, detailing the magnitude of nosocomial infections and strategies to prevent the spread of infections in healthcare settings. It emphasizes the importance of standard precautions, proper hand hygiene, use of personal protective equipment (PPE), and effective waste management to protect patients, healthcare workers, and the community. The guidelines aim to make healthcare facilities safer by reducing the risk of infection and promoting health education.