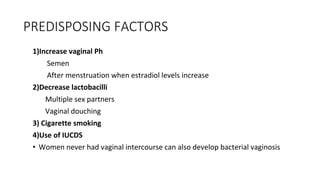
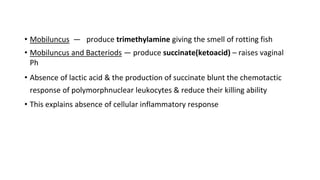
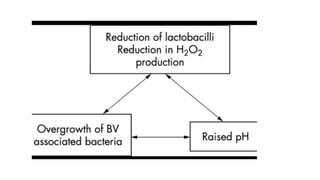
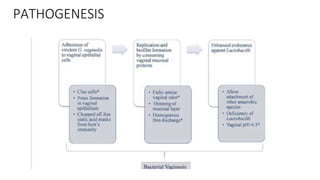
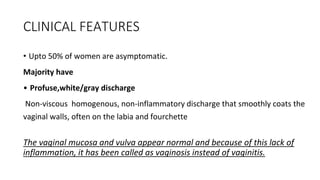
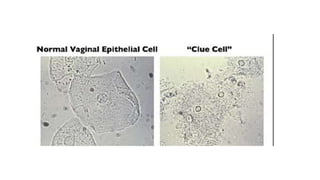
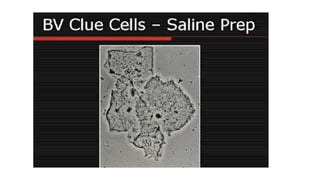
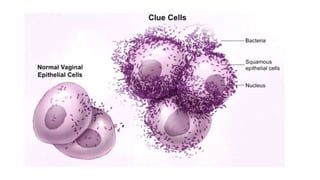
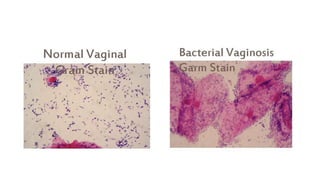
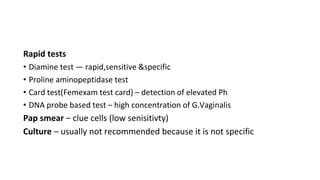
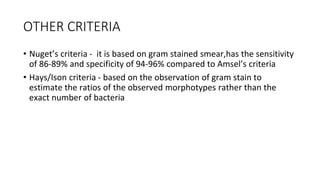
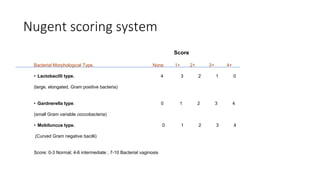
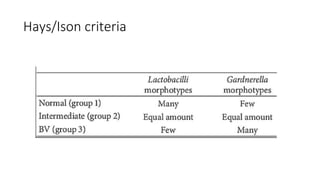
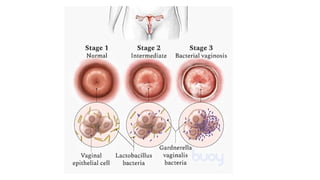
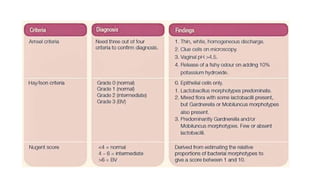
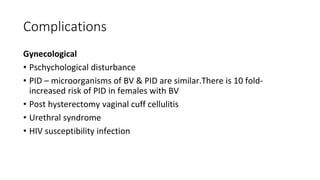
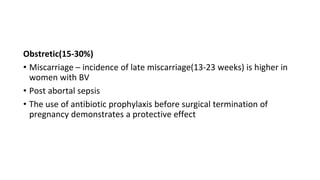
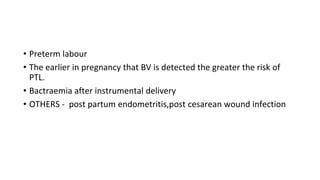
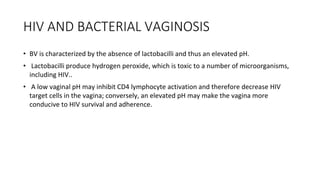
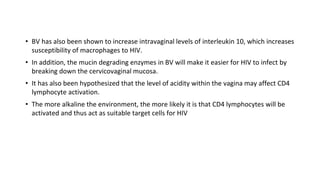
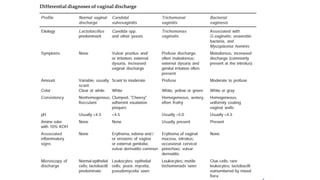
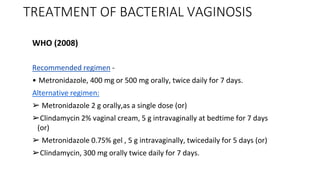
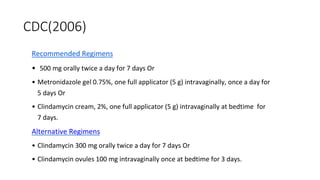
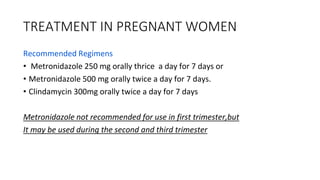
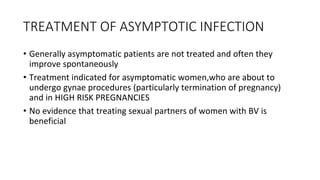
Bacterial vaginosis is a common cause of abnormal vaginal discharge and odor in women. It occurs when the normal vaginal bacteria, predominantly lactobacillus, are replaced by an overgrowth of anaerobic bacteria. This causes the vaginal pH to increase, resulting in a grayish white discharge with a fishy odor. Bacterial vaginosis increases the risk of complications during pregnancy like preterm birth and miscarriage. It is diagnosed using Amsel's criteria which looks for clue cells on microscopy and a high vaginal pH. Treatment involves oral or topical antibiotics like metronidazole or clindamycin.