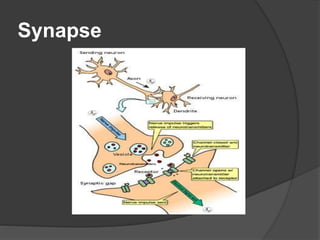
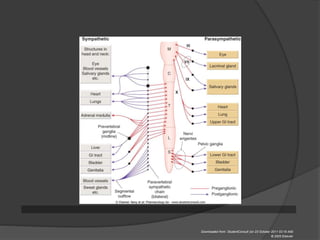
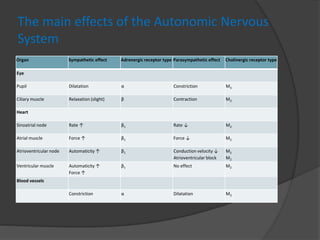
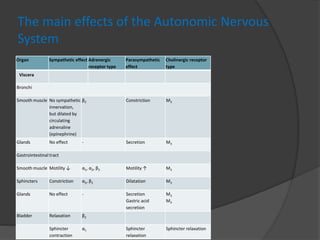
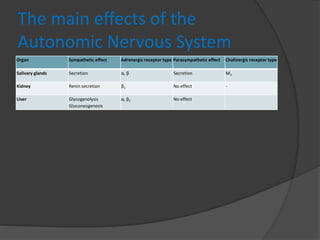
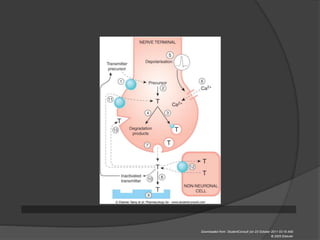
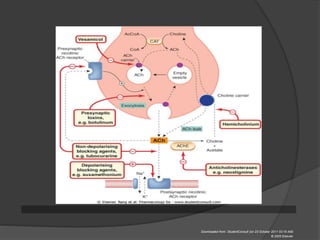
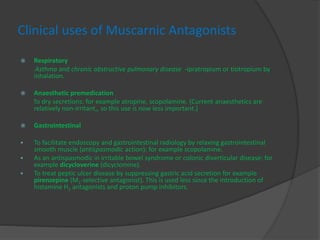
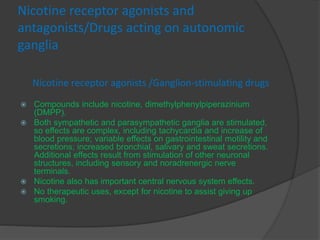
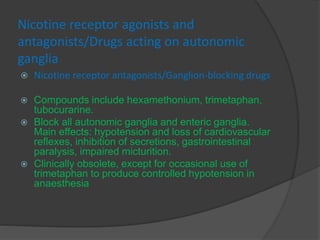
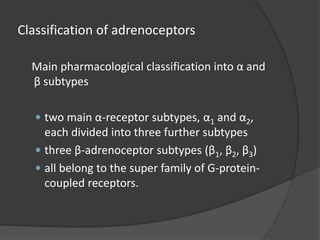
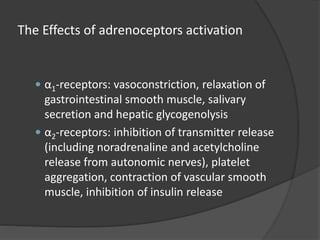
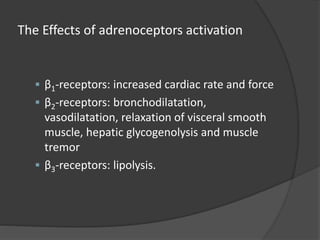
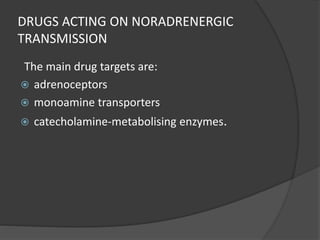
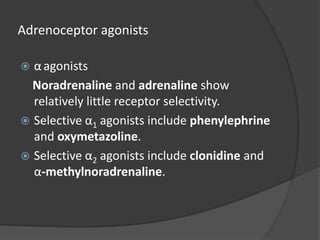
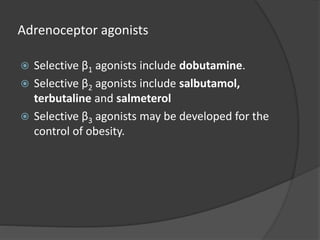
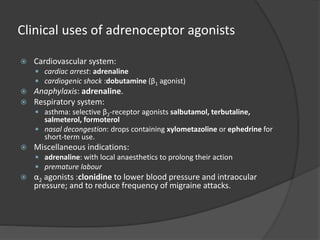
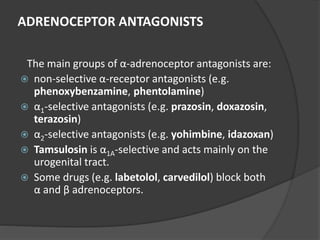
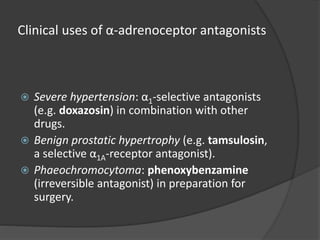
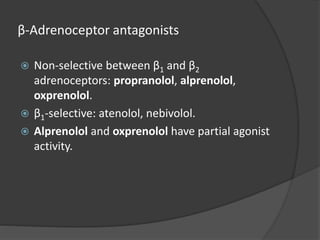
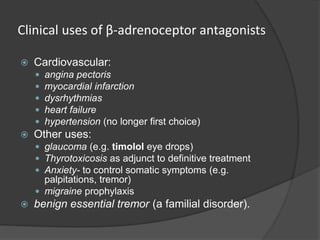
The document discusses synapses and the autonomic nervous system. It describes two types of synapses - chemical and electrical. The autonomic nervous system consists of the sympathetic and parasympathetic systems which regulate organs through the release of neurotransmitters like acetylcholine and norepinephrine. The effects of these systems are described for various organs. Drugs can act as agonists or antagonists at cholinergic and adrenergic receptors to influence the autonomic nervous system.