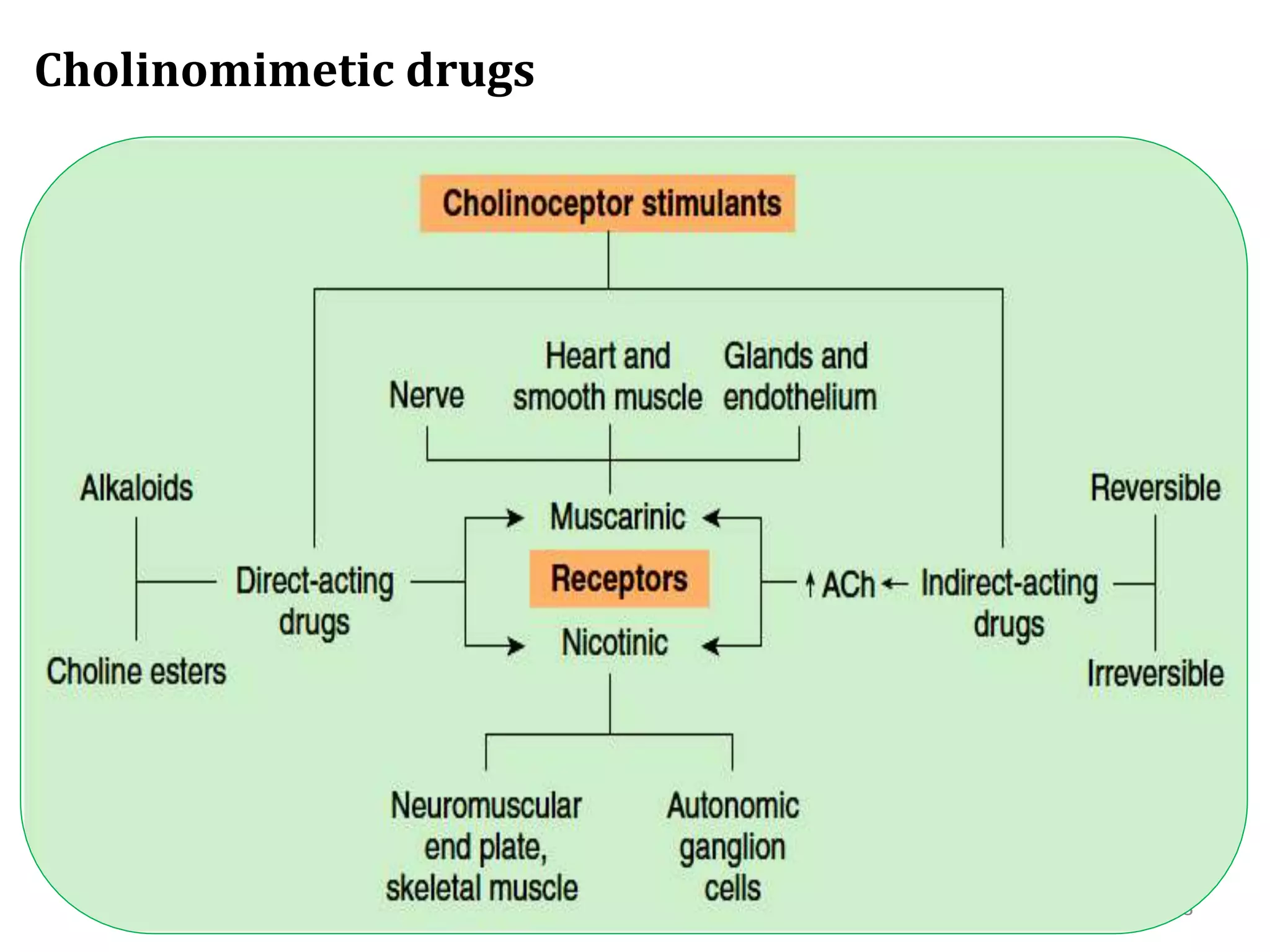
This document discusses the autonomic nervous system. It begins by defining the somatic and autonomic nervous systems, and their components. It then compares the somatic and autonomic nervous systems. The functions of the sympathetic and parasympathetic nervous systems are described. Cholinergic and adrenergic receptors are explained. The document concludes by discussing cholinergic and adrenergic drugs, including their classifications, mechanisms of action, uses and side effects.


















































![ -Blockers
A. Non selective -Blockers
– Are also called 1st generation -blockers
– Propranolol, Timolol, Nadolol, Pindolol
B. Cardio selectives [1Blockers ]
– Are called 2nd generation -blockers
– Atenolol, Bisoprolol, Esmolol, Metoprolol
C. Non-selective adrenergic blockers( & Blockers)
– Are also called 3rd generation -blockers
– Carvedilol, Labetalol, Bucindolol, Nebivolol
Longest half life: Nadolol, Cartelol (24 hrs)
Shortest half life: Esmolol (10 min) 53](https://image.slidesharecdn.com/22-230218170117-c5fd9e68/75/22-ANS-Pharmacology-pptx-53-2048.jpg)






