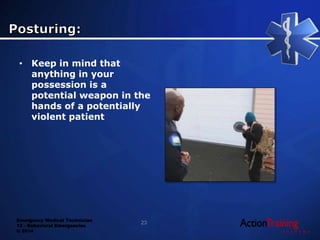
This document discusses behavioral emergencies and how to handle them as an EMT. It covers potential causes of behavioral issues like medical conditions, substance abuse, and psychiatric conditions. It emphasizes the importance of assessing for risks, maintaining safety, and looking for underlying medical problems. Specific situations covered include suicide risk assessment, substance abuse including stimulants, depressants, hallucinogens, and inhalants, and providing emergency medical care for behavioral emergency patients.