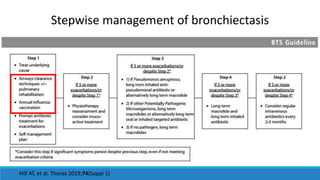
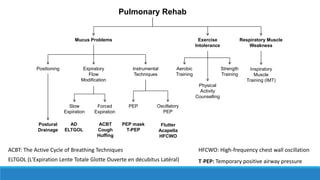
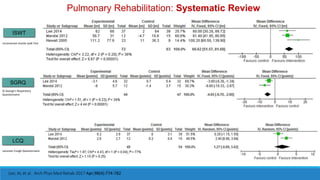
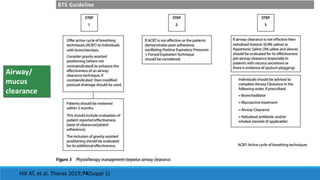
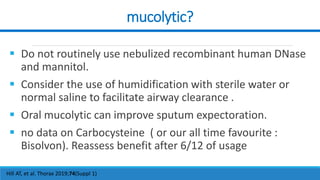
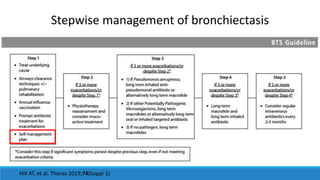
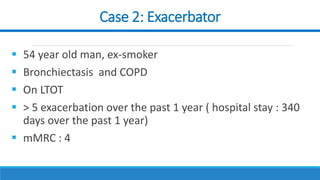
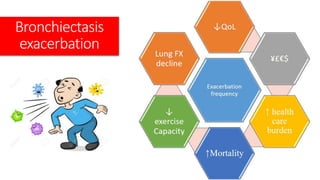
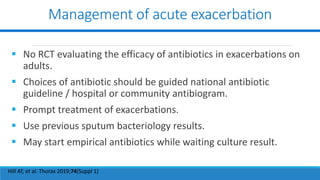
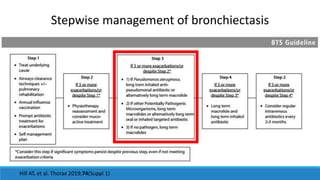
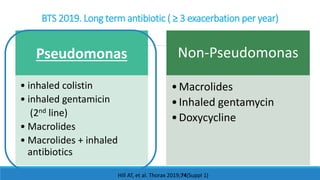
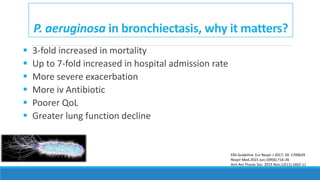
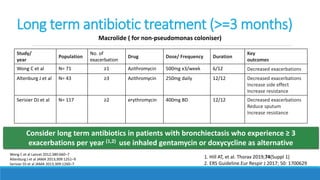
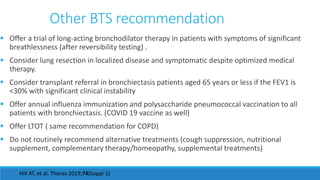
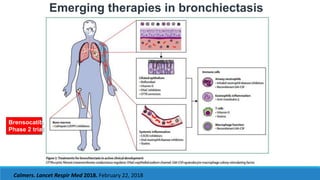
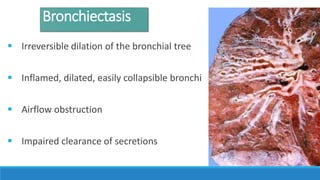
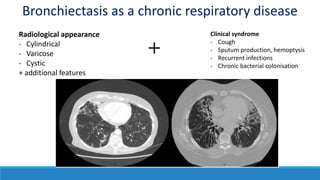
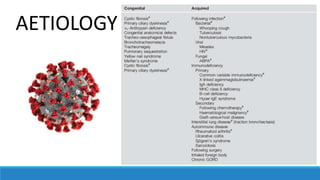
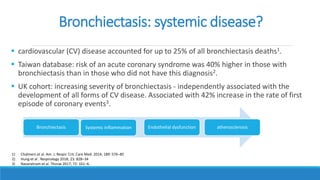
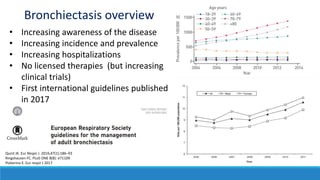
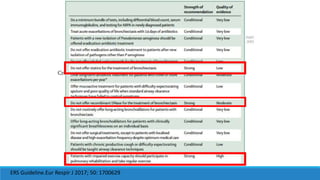
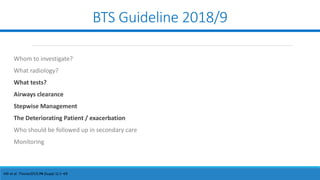
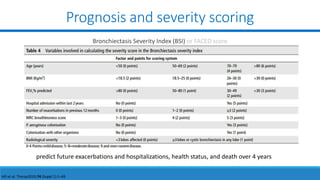
This document provides an overview and management guidelines for bronchiectasis. It begins with definitions and descriptions of bronchiectasis, including its clinical presentation and radiological appearance. It then discusses current understanding of bronchiectasis as a systemic disease associated with increased cardiovascular risk. Guidelines for diagnosis and assessment of severity from the British Thoracic Society are summarized. The document presents two clinical cases and reviews recommendations for management of stable disease and exacerbations, including airway clearance techniques, antibiotics, pulmonary rehabilitation, and emerging therapies.


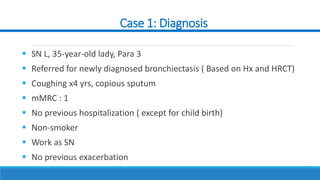


![Case 1: SN L
BMI: 23. FBC: TWC; 6.2 (eosinophil : 9.9%[0.6]), Hb: 11, PLT: 318
RP/ LFT/ FBS: normal
Sputum MTB x2 : negative
Sputum Culture: no growth
RF/ ANCAs/ ANA: -ve
IgG, IgM, IgA: normal level. Serum Galactomannan: -ve
Spirometry 24/5/19:
FEV1: 2.31L (70% pred)
FVC: 2.87L (72% pred)
FEV1/FVC: 80%
BSI: 1 (MILD)
Complaint of copious sputum, through out the day, interfering her job as nurse.](https://image.slidesharecdn.com/bronchiectasisapulmonaryandsystemicdisease2022-220905100304-b5357b5f/85/bronchiectasis-a-pulmonary-and-systemic-disease-2022-pptx-18-320.jpg)