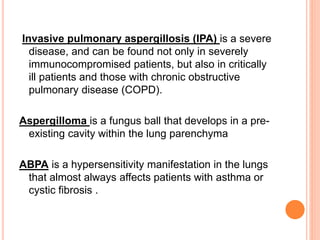
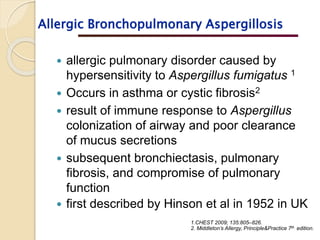
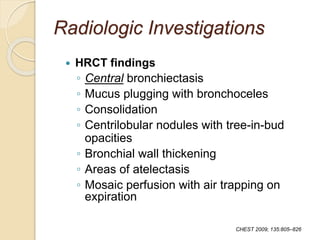
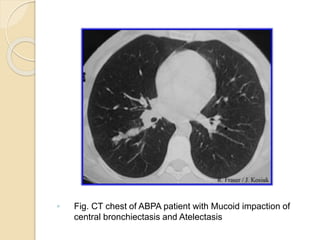
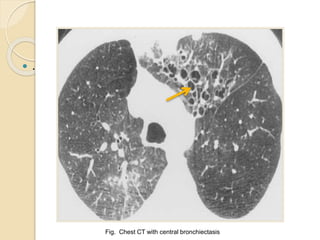
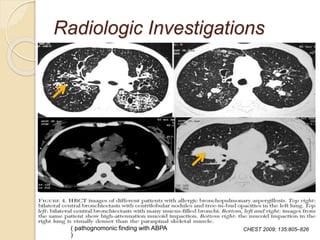
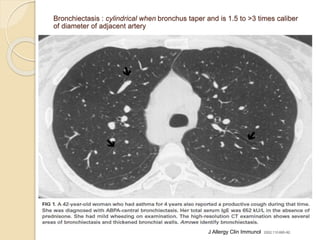
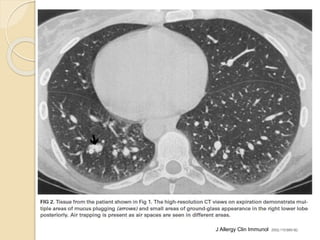
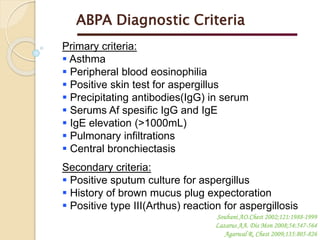
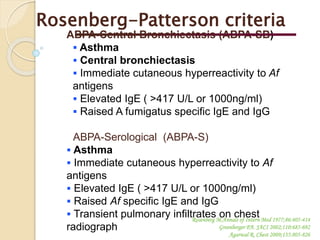
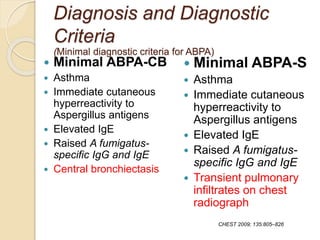
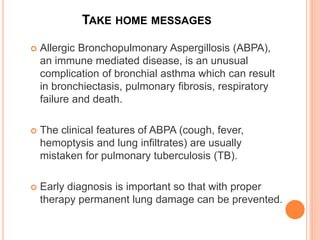
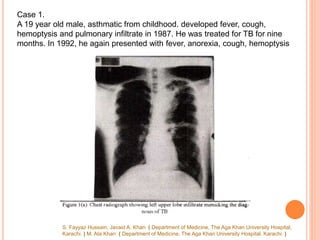
The document outlines two case studies of allergic bronchopulmonary aspergillosis (ABPA) in asthmatic patients, detailing symptoms, diagnosis, and treatment outcomes. It indicates ABPA's prevalence among asthmatics and notes many cases are misdiagnosed as pulmonary tuberculosis, emphasizing the need for better diagnostic protocols. The documentation also discusses the laboratory findings, radiologic features, and diagnostic criteria for ABPA, highlighting its association with asthma and potential complications.
![CHEST. 2006;130(2):442-448. DOI:10.1378/CHEST.130.2.442
ALLERGIC BRONCHOPULMONARY ASPERGILLOSIS*:LESSONS FROM 126
PATIENTS ATTENDING A CHEST CLINIC IN NORTH INDIA.
RITESH AGARWAL, MD, DM, FCCP; DHEERAJ GUPTA, MD, DM, FCCP; ASHUTOSH N. AGGARWAL, MD, DM;
DIGAMBER BEHERA, MD, FCCP; SURINDER K. JINDAL, MD, FCCP
Five hundred sixty-four patients were screened using an Aspergillus skin test; 223 patients (39.5%)
were found to be positive, and ABPA was diagnosed in 126 patients (27.2%). There were 34 patients
(27%) with ABPA-S, 42 patients with ABPA-CB, and 50 patients with ABPA-CB-ORF. Fifty-nine patients
(46.8%) had received antitubercular therapy in the past. The vast majority of patients had bronchiectasis
at presentation to our hospital. High-attenuation mucous impaction was noted in 21 patients (16.7%).
There was no significant difference between the stages of ABPA and the duration of illness, the severity
of asthma, and the serologic findings (ie, absolute eosinophil count, IgE levels [total] and IgE levels
[for Aspergillus fumigatus]).
Conclusions: There is a high prevalence of ABPA in asthmatic patients presenting at our hospital. The
disease entity is still underrecognized in India; the vast majority of patients
have bronchiectasis at presentation, and almost half are initially
misdiagnosed as having pulmonary tuberculosis. There is a need to redefine the
definitions of ABPA and the optimal dose/duration of glucocorticoid therapy. This study reinforces the
need for the routine screening of asthmatic patients with an Aspergillus skin test.
Fifty-nine patients (46.8%) had received antitubercular therapy in the past](https://image.slidesharecdn.com/abpa-151213033418/85/Abpa-a-diagnostic-dilemma-10-320.jpg)
![ 17. D´Urzo,Mclvor A.R. Allergic bronchopulmonary aspergillosis in asthma.
Can Fam Physician. 2000 Apr; 46: 882–884.
18. Shah A, Panchal N, Agarwal AK. Concomitant allergic bronchopulmonary
aspergillosis and allergic aspergillus sinusitis: a review of an uncommon
association. Clin Exp Allergy 2001;31:1896–1905. [CrossRef] [Medline]
19. Agarwal R, Srinivas R, Jindal SK. Allergic bronchopulmonary aspergillosis
complicating chronic obstructive pulmonary disease. Mycoses 2007;51:83–85.
20. Boz AB, Celmeli F, Arslan AG, Cilli A, Ogus C, Ozdemir T. A case of allergic
bronchopulmonary aspergillosis following active pulmonary
tuberculosis. Pediatr Pulmonol 2009;44:86–89. [CrossRef] [Medline]
21. Judson MA. Allergic bronchopulmonary aspergillosis after infliximab therapy
for sarcoidosis: a potential mechanism related to T-helper cytokine
balance. Chest 2009;135:1358–1359. [CrossRef] [Medline]
39. Agarwal R, Singh N, Gupta D. Pulmonary hypertension as a presenting
manifestation of allergic bronchopulmonary aspergillosis. Indian J Chest Dis Allied
Sci 2009;51:37–40. [Medline]
Uncommon associations of allergic bronchpulmonary aspergillosis](https://image.slidesharecdn.com/abpa-151213033418/85/Abpa-a-diagnostic-dilemma-16-320.jpg)