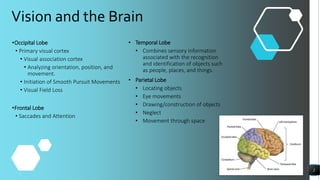
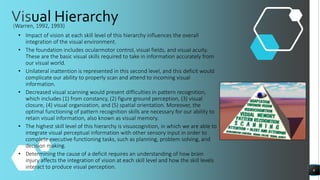
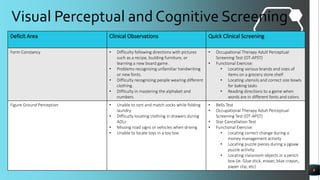
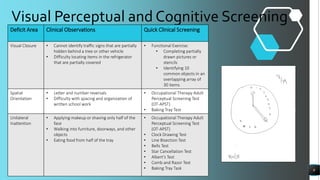
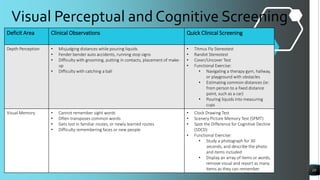
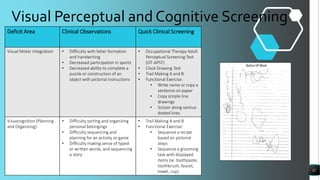
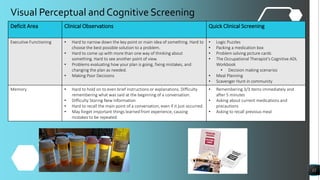
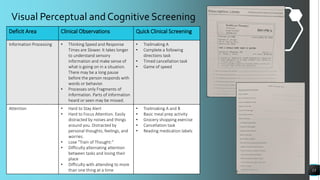
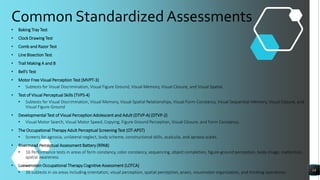
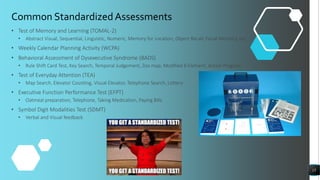
The document discusses evaluation and treatment of visual perception and cognition following brain injury. It begins by outlining the brain regions involved in vision and visual processing. It then defines key terms related to visual perception. The objectives are to improve understanding of evaluation, treatment techniques, and the impact on everyday functioning. Evaluation involves screening visual skills and perceptual processes. A visual hierarchy is described showing how skills build upon each other. Specific screening tools and exercises are provided to assess processes like form constancy, figure-ground perception, and unilateral neglect. The summary highlights the main topics and goals covered in the document.













![References Continued
• 49. Tinelli F, Cioni G, Purpura G. Development and implementation of a new telerehabilitation system for audiovisual stimulation training in hemianopia. Front Neurol. 2017;8(621), 1-10. doi:10.3389/fneur.2017.00621
• 50. Frassinetti F, Bolognini N, Bottari D, Bonora A, Ladavas E. Audiovisual integration in patients with visual deficit. J Cogn Neurosci. 2005; 17(9), 1442-1452. doi:10.1162/0898929054985446
• 51. Makovski T. The open-object illusion: Size perception is greatly influenced by object boundaries. Atten Percept Psychophys. 2017; 79, 1282-1289. doi:10.3758/s13414-017-1326-5
• 52. Kalloniatis M, Luu C. The Perception of Depth. 2005 May 1 [Updated 2007 Jun 6]. In: Kolb H, Fernandez E, Nelson R, editors. Webvision: The Organization of the Retina and Visual System [Internet]. Salt Lake City (UT): University of Utah Health Sciences Center; 1995.
Accessed July 26, 2018.
• 53. Gillen G. Cognitive and perceptual rehabilitation: optimizing function. St. Louis, MO.: Mosby/ELSEVIER; 2009.
• 54. Appelros P, Karlsson GM, Thorwalls A, Tham K, Nydevik I. Unilateral neglect: further validation of the baking tray task. J Rehabil Med. 2004;36(6):258-261. Retrieved September 7, 2018. doi:10.1080/16501970410029852
• 55. Bailey M, Riddoch J, Crome P. Test-retest stability of three tests for unilateral visual neglect in patients with stroke: Star Cancellation, Line Bisection, and Baking Tray Task. Neurospychol Rehabil, 2004; 14(4), 403-419. doi:10.1080/09602010343000282
• 56. Allen D, Thaler N, Ringdahl EN, Mayfield J. Comprehensive trail making test performance in children and adolescents with traumatic brain injury. Psychol Assess. 2011; (24): 556-564. doi:10.1037/a0026263
• 57. Desrosiers G, Kavanagh D. Cognitive assessment in closed head injury: stability, validity, and parallel forms for two neuropsychological measures of recovery. Int J Clin Neuorpsychol. 1987; 9(4), 162-173. Retrieved July 26, 2018.
• 58. Sanchez-Cubillo, I, Perianez, J, Adrover-Roig, D, et al. Construct validity of the Trail Making Test: role of task-switching, working memory, inhibition/interference control, and visuomotor abilities. J Int Neuropsychol Soc. 2009;15(3), 438. doi:10.1017/S1355617709090626
• 59. Gauthier L, Dehaut F, Joanette Y. The Bells Test: a quantitative and qualitative test for visual neglect. Int J Clin Neuropsychol, 1989;(11), 49-54. Retrieved July 26, 2018.
• 60. Ferber S, Karnath HO. How to assess spatial neglect–Line Bisection or Cancellation Tests? J Clin Expl Neuropsychol, 2001;(23), 599-607. doi:10.1076/jcen.23.5.599.1243
• 61. Brown TG, Rodger S, Davis A. Motor-Free Visual Perception Test – Revised: An overview and critique. British Journal of Occupational Therapy. 2003;66(4), 159-167. doi:10.1177/030802260306600405
• 62. McKenna K, Cooke D, Fleming J, Jefferson A, Ogden S. The incidence of visual perceptual impairment in patients with severe traumatic brain injury. Brain Inj. 2006;20(5), 507-518. doi:10.1080/02699050600664368
• 63. Cooke DM, McKenna K, Fleming J, Darnell.R. Criterion validity of the Occupational Therapy Adult Perceptual Screening Test (OT-APST). Scand J Occup Ther. 2006;13(1), 38-48, doi:10.1080/11038120500363006
• 64. Cooke DM, McKenna K, Fleming J, Darnell R. Australlian normative data for the occupational therapy adult perceptual screening test. Aust Occup Ther J. 2006; (53), 325-336. doi:10.1111/j.1440-1630.2006.00597.x
• 65. Friedman PJ, Leong L. The rivermead perceptual assessment battery in acute stroke. Br J Occup Ther. 1992;55(6): 233-237. doi:10.1177/030802269205500608
41](https://image.slidesharecdn.com/assessmentandinterventionofvisualperceptionandcognition3-230518224430-24fd5746/85/Assessment_and_Intervention_of_Visual_Perception_and_Cognition3-pdf-41-320.jpg)