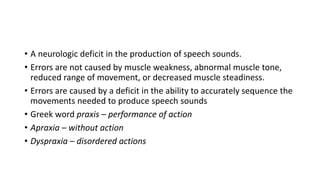
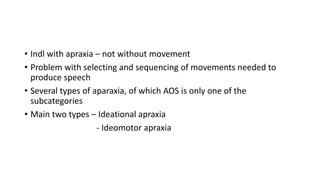
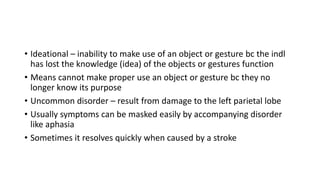
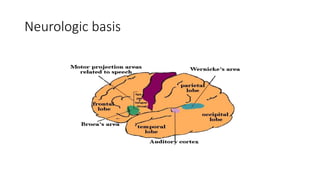
This document discusses apraxia of speech (AOS), which is a neurologic disorder characterized by a deficit in the ability to accurately sequence movements needed to produce speech sounds. It is caused by damage to areas involved in motor planning and programming of speech, particularly in the left frontal lobe near Broca's area. The document outlines different types of apraxia, including ideational apraxia which affects object use due to loss of knowledge, and ideomotor apraxia which disrupts voluntary movements. AOS is a subtype of ideomotor apraxia that specifically impacts phoneme production. Common causes of AOS include strokes, degenerative diseases, and traumatic brain injuries affecting the left perisylvian region