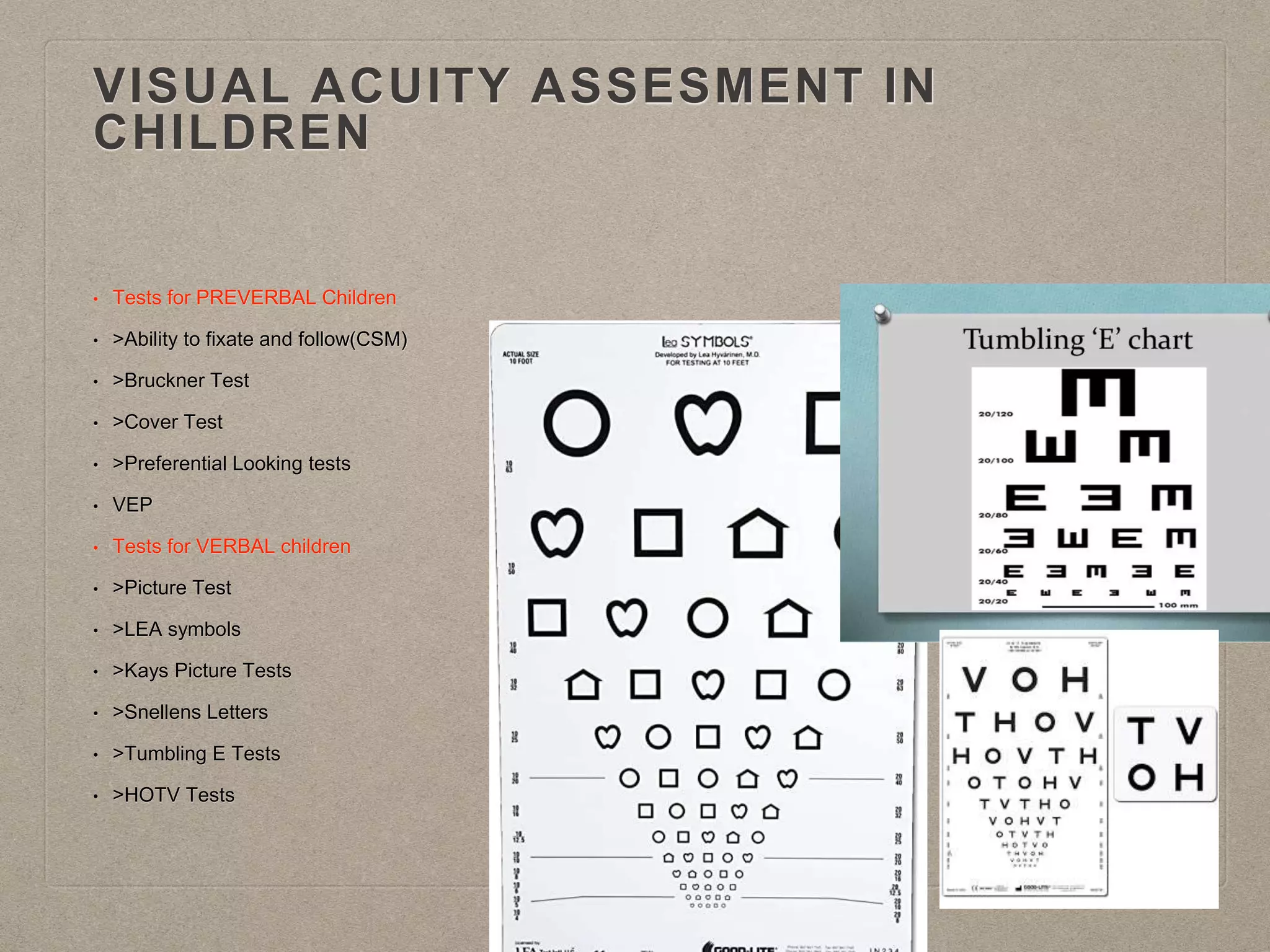
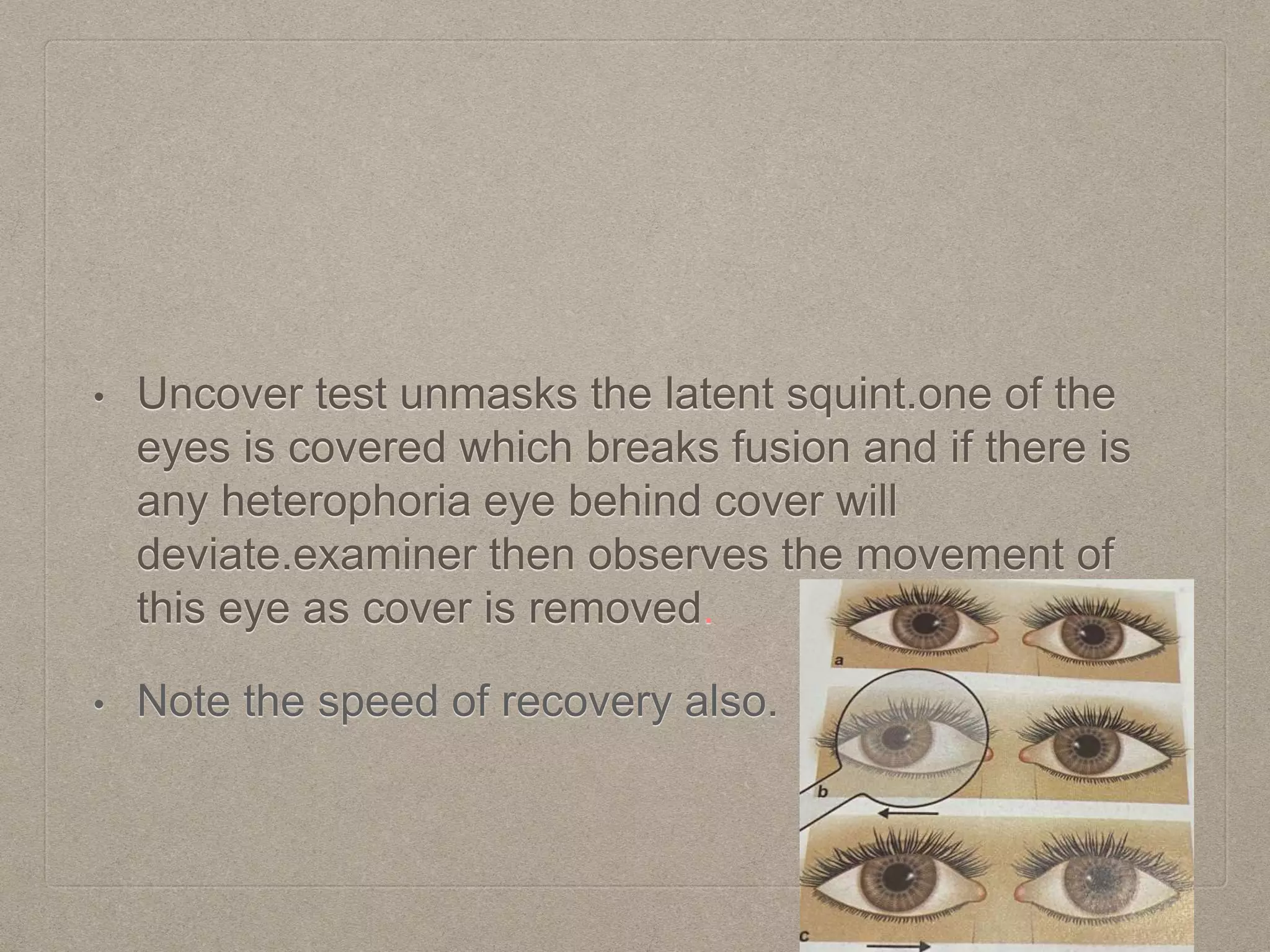
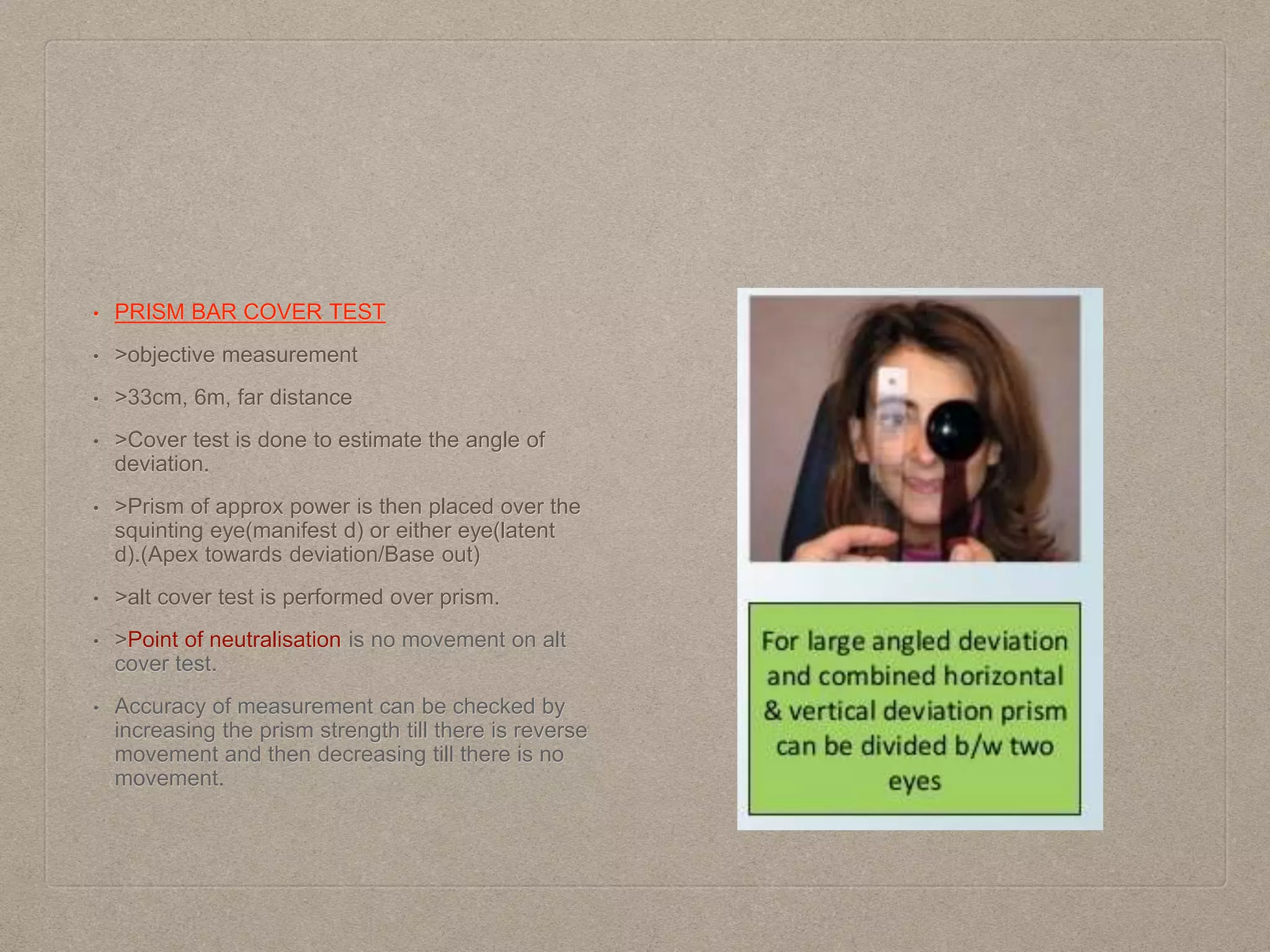
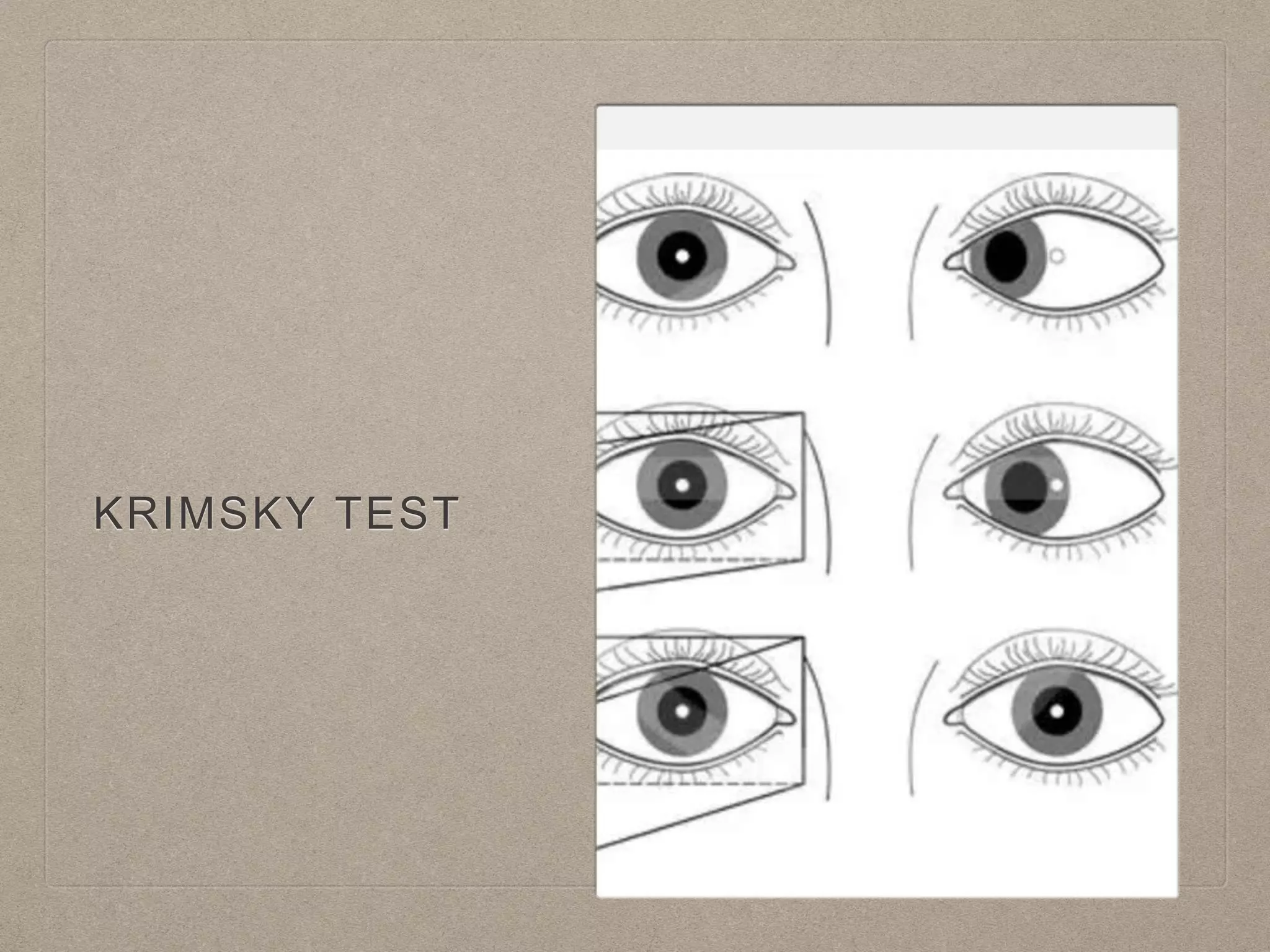
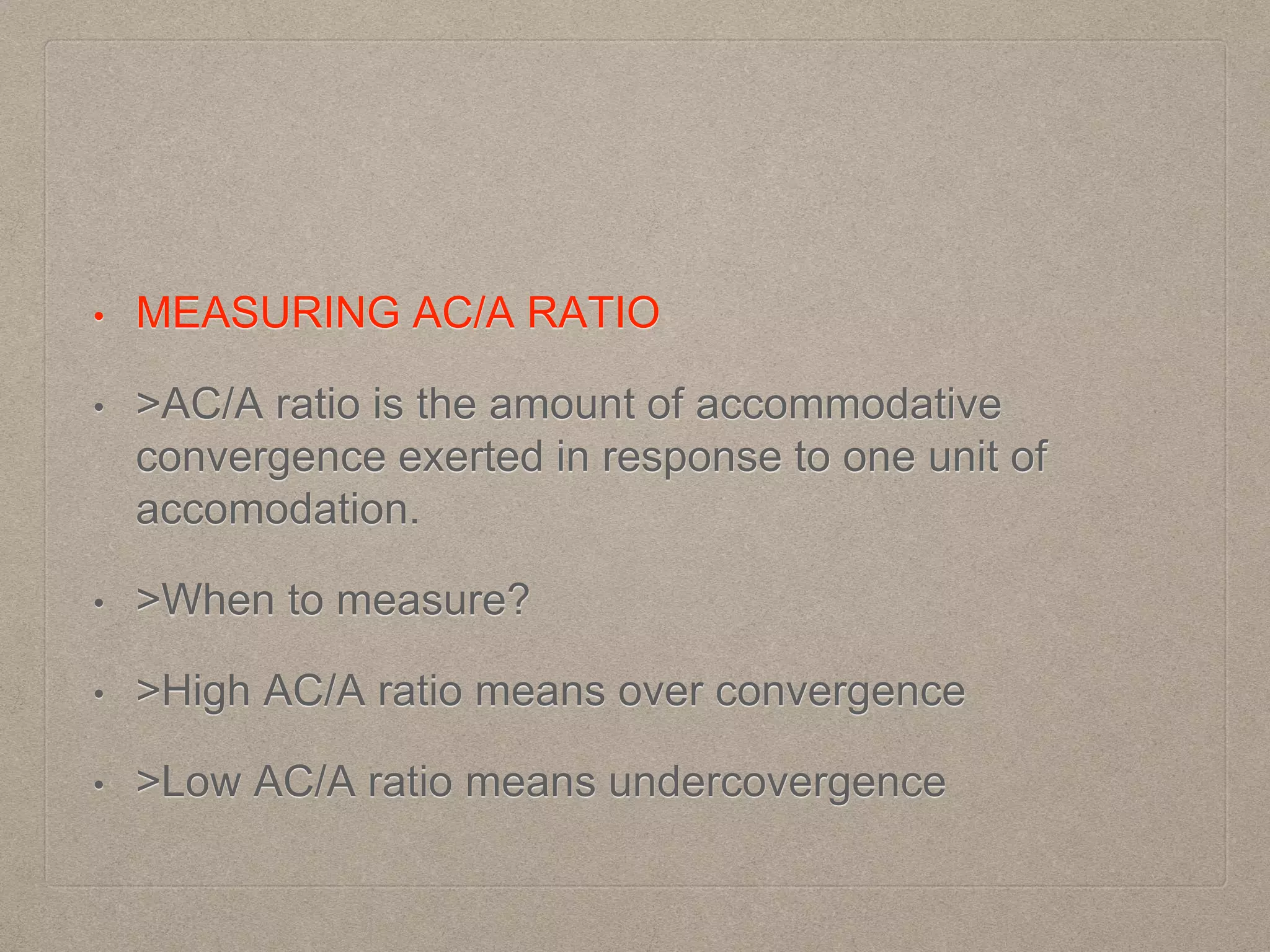
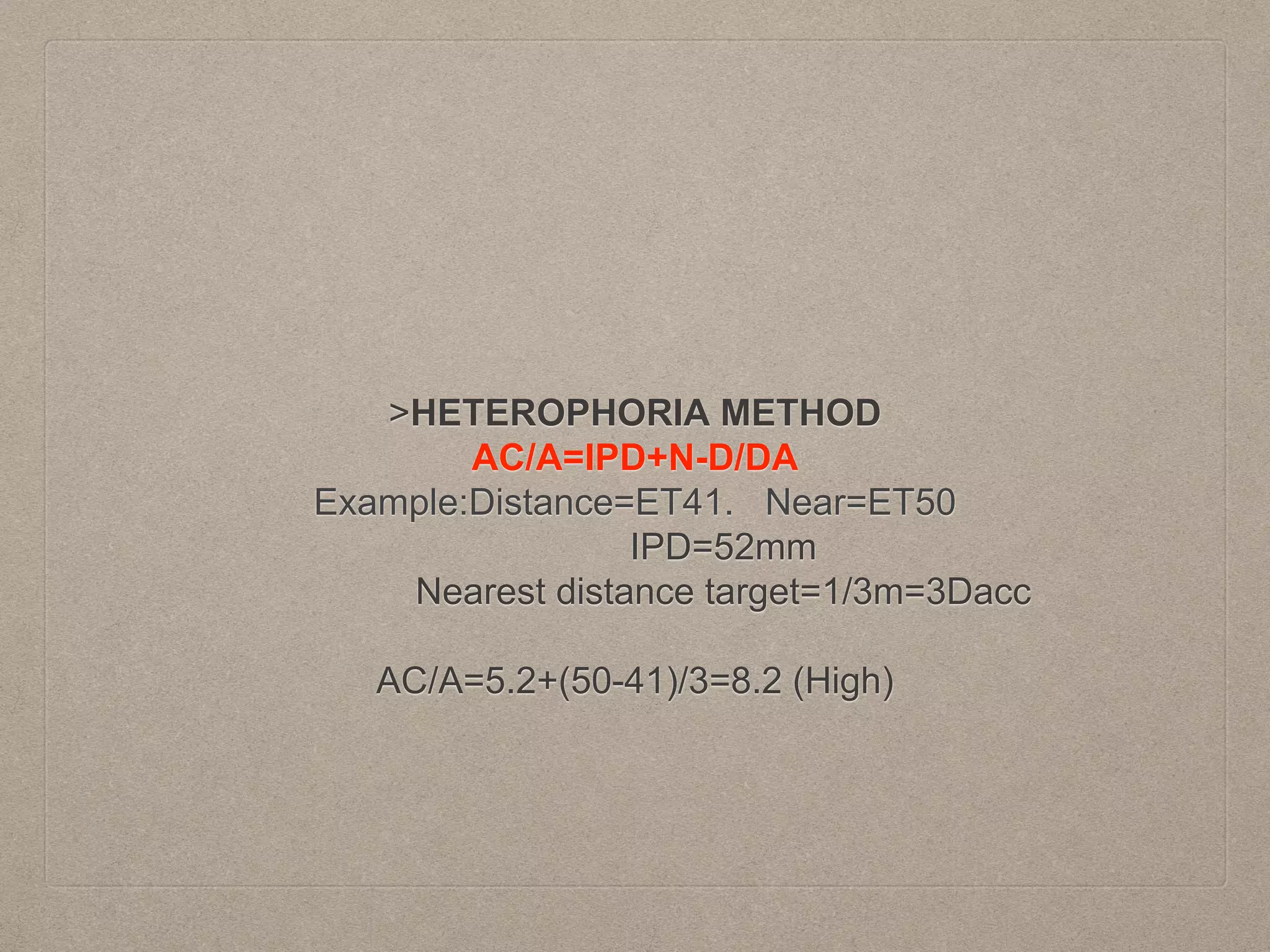
This document provides guidance on examining a patient with strabismus. It outlines the goals of assessment as well as techniques for taking a thorough history, measuring eye alignment and movements, assessing binocular vision status, and performing supplementary tests. Key parts of the exam include visual acuity testing, inspection of eye position and movements, motor testing using cover-uncover and prism bar tests, sensory evaluation for diplopia and suppression, and testing for stereopsis. The order of examination and interpretation of test results are also discussed to establish a diagnosis and guide management.