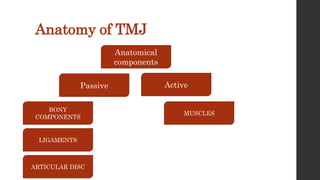
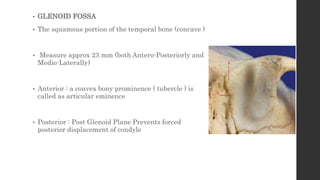
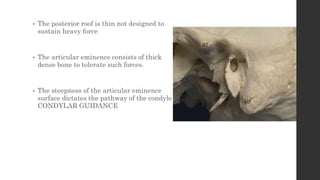
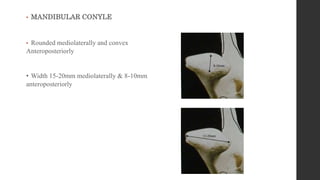
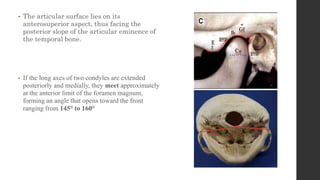
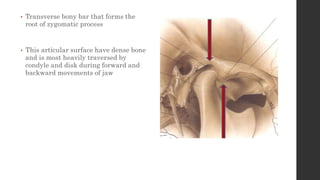
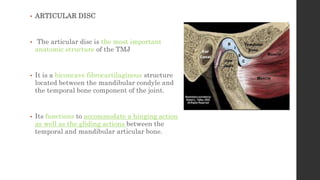
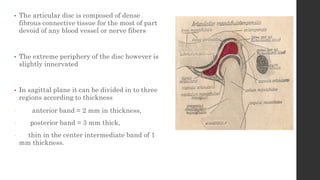
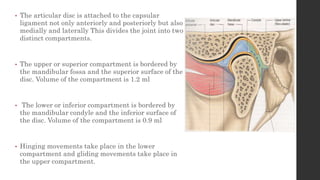
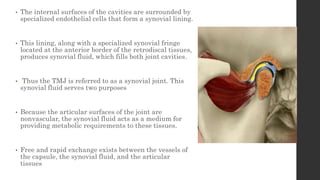
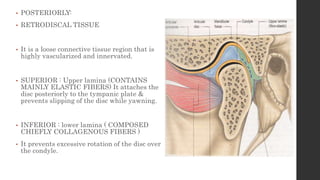
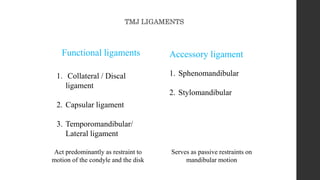
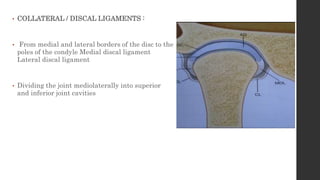
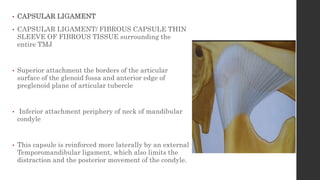
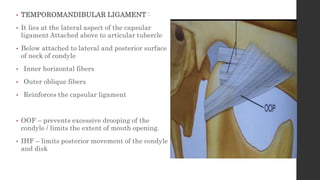
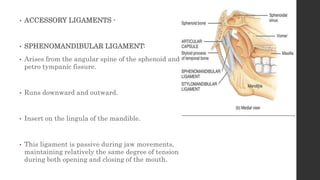
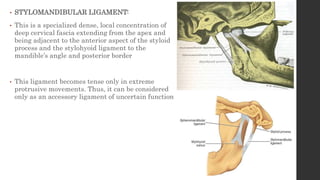
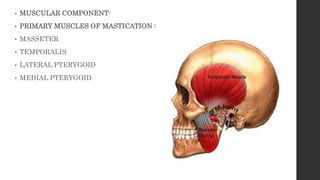
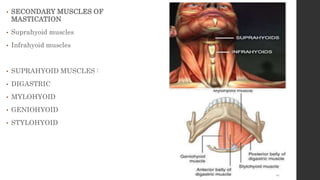
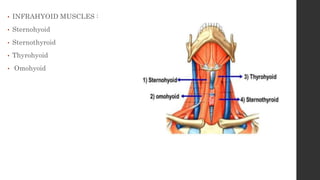
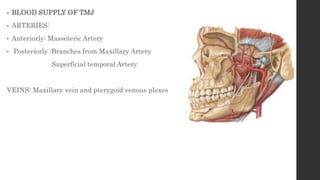
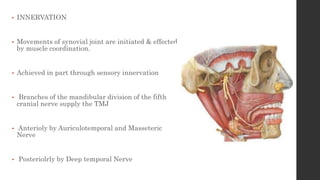
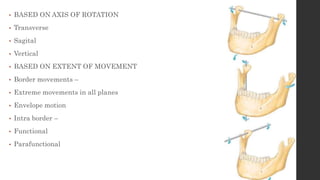
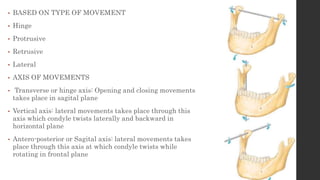
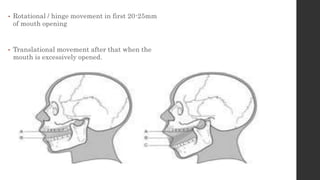
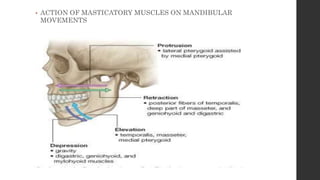
The document summarizes the anatomy and movements of the temporomandibular joint (TMJ). It describes the bony components, articular disc, ligaments, muscles, blood supply, and nerve supply of the TMJ. It also discusses the different types of mandibular movements including hinge, protrusive, retrusive, and lateral movements as well as habitual movements like speech, mastication, and deglutition. The TMJ allows hinging and gliding movements of the mandible for functions like eating and talking.