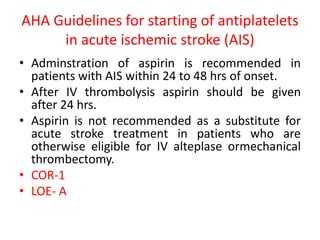
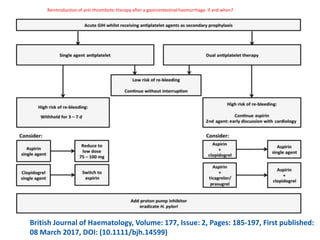
- Aspirin is recommended within 24-48 hours for acute ischemic stroke (AIS) and after 24 hours if IV thrombolysis is administered.
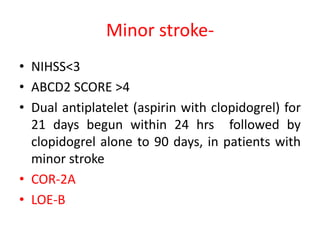
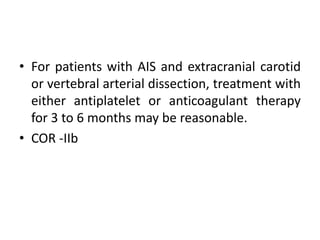
- For minor strokes, dual antiplatelet therapy with aspirin and clopidogrel for 21 days begun within 24 hours is recommended, followed by clopidogrel alone for 90 days.
- The efficacy of IV antiplatelet drugs like tirofiban and eptifibatide for AIS is not well established and requires further research.