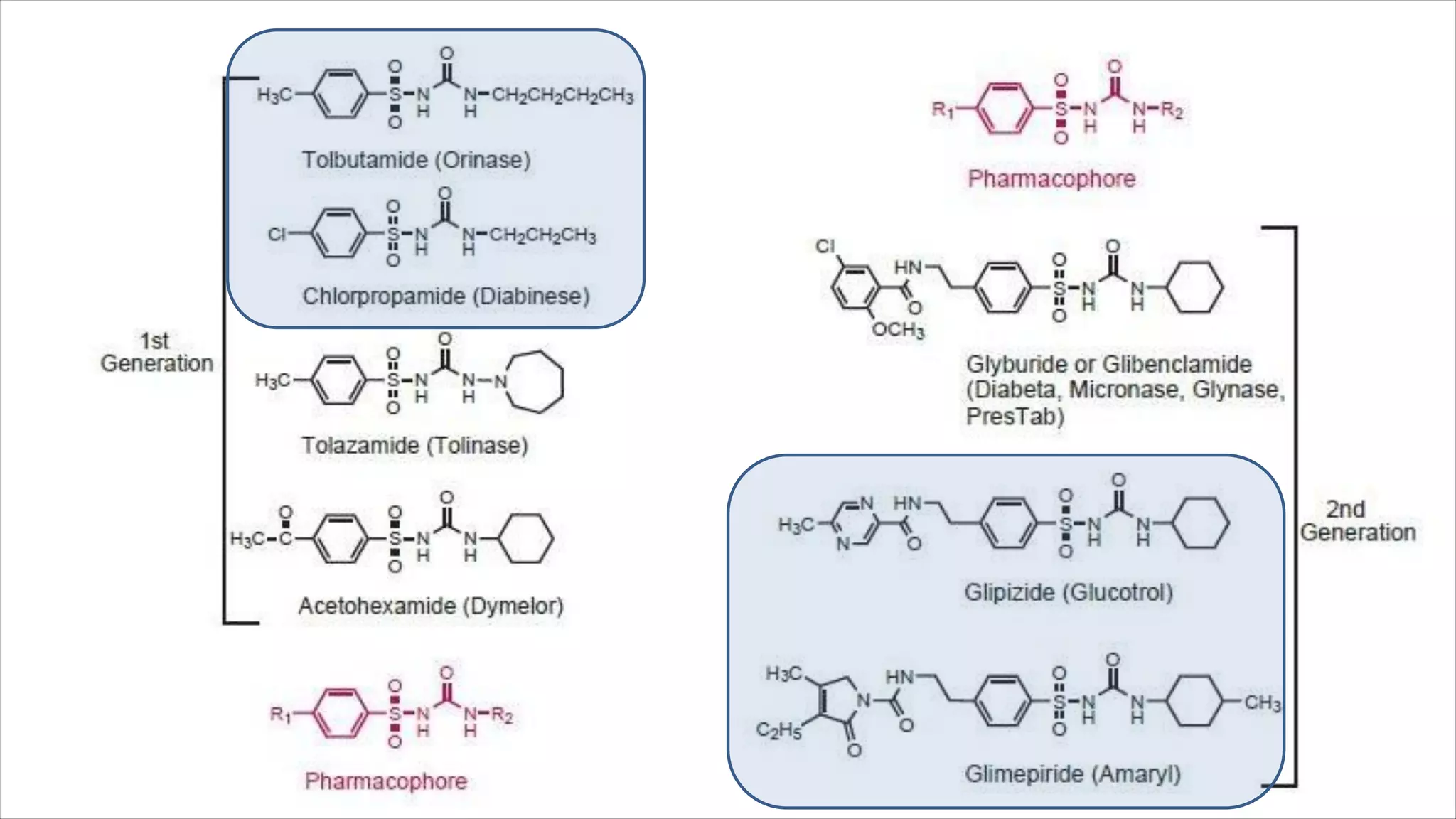
The document discusses various classes of antidiabetic agents including insulin and its preparations, sulfonylureas, biguanides, thiazolidinediones, meglitinides, and glucosidase inhibitors. It provides details on the mechanisms of action, metabolism and effects of representative drugs from each class such as glimepiride, glargine, repaglinide, pioglitazone and metformin. The classes of drugs work by various mechanisms including stimulating insulin release, increasing insulin sensitivity, suppressing glucose production or slowing glucose absorption.




![Tolbutamide
1-butyl-3-(p-tolylsulfonyl)urea
Chlorpropamide
1-[(p-chlorophenyl)-sulfonyl]-3-propylurea
This drug is more resistant to conversion to
inactive metabolites than is tolbutamide and, as a
result, has a much longer duration of action.
One study showed that about half of the drug is
excreted as metabolites, with the principal one
being hydroxylated (ω and ω-1) in the 2-position
of the propyl side chain.](https://image.slidesharecdn.com/antidiabetic-221004105026-95a8a725/75/Antidiabetic-pdf-14-2048.jpg)
![Glipizide: 1-cyclohexyl-3-[[p-(2-(5-methylpyrazinecarboxamido) ethyl]phenyl]sulfonyl]urea is a
cyclohexylsulfonylurea analog similar to acetohexamide and glyburide, with a pKa of 5.9.
Metabolism of glipizide is generally through
oxidation of the cyclohexane ring to the p-hydroxy
and m-hydroxy metabolites.
A minor metabolite that occurs involves the
N - acetyl derivative, which results f rom the
acetylation of the primary amine following hydrolysis
of the amide system by amidase enzymes.
2nd GENERATION](https://image.slidesharecdn.com/antidiabetic-221004105026-95a8a725/75/Antidiabetic-pdf-15-2048.jpg)

![Glimepiride:
1-[[p-[2-(3-ethyl-4-methyl-2-oxo-3-
pyrroline-1-carboxamido)ethyl]phenyl]
sulfonyl]- 3-(trans-4-methylcyclohexyl)
urea, is very similar to glipizide with the
exception of their heterocyclic rings.
Instead of the pyrazine ring found in
glipizide, glimepiride contains a
pyrrolidine system.
It is metabolized primarily through
oxidation of the alkyl side chain of the
pyrrolidine, with a minor metabolic route
involving acetylation of the amine.](https://image.slidesharecdn.com/antidiabetic-221004105026-95a8a725/75/Antidiabetic-pdf-17-2048.jpg)

![Repaglinide: (+)-2-ethoxy-4-[N-[3- methyl- 1( S)-[ 2-( 1
piperidinyl) phenyl] butyl]carbamoyl-methyl]benzoic acid
represents a new class of nonsulfonylurea oral hypoglycemic
agents. With a fast onset and a short duration of action, the
medication should be taken with meals.
N a t e g l i n i d e : A l t h o u g h n a t e g l i n i d e , N-( 4
isopropylcyclohexanecarbonyl)- D-phenylalanine, belongs to
the metaglinides, it is a phenylalanine derivative and represents
a novel drug in the management of type 2 diabetes.
It is oxidized by CYP 3A4, and the carboxylic acid may be
conjugated to inactive compounds. Less than 0.2% is
excreted unchanged by the kidney, which may be an
advantage for elderly patients who are renally impaired.
The most common side effect involves hypoglycemia, resulting in shakiness, headache, cold sweats,
anxiety, and changes in mental state.](https://image.slidesharecdn.com/antidiabetic-221004105026-95a8a725/75/Antidiabetic-pdf-22-2048.jpg)
![Thiazolindiones (TZD)
INSULIN SENSITIZERS, PEROXISOME PROLIFERATOR
ACTIVATED RECEPTOR [PPAR] AGONISTS, GLITAZONES](https://image.slidesharecdn.com/antidiabetic-221004105026-95a8a725/75/Antidiabetic-pdf-23-2048.jpg)



![Rosiglitazone: 5-[4-[2-(N-methyl-N-(2-pyridyl)amino)ethoxy]
benzyl] thiazolidine-2,4-dione.
The major routes of biotransformation are N-demethylation and
hydroxylation of the pyridine ring p
a
a
r to the amino nitrogen,
with CYP2C8.](https://image.slidesharecdn.com/antidiabetic-221004105026-95a8a725/75/Antidiabetic-pdf-29-2048.jpg)
![Pioglitazone: 5-(4-[2-(5-ethylpyridin- 2-
yl)ethoxy]benzyl)thiazolidine-2,4-dione, the
compound is used as the racemic mixture.
This is primarily a result of the in vivo
interconversion of the two enantiomers. Thus,
there are no differences in the pharmacological
activity of the two enantiomers.](https://image.slidesharecdn.com/antidiabetic-221004105026-95a8a725/75/Antidiabetic-pdf-30-2048.jpg)