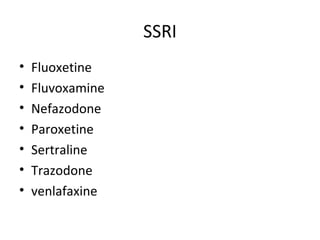
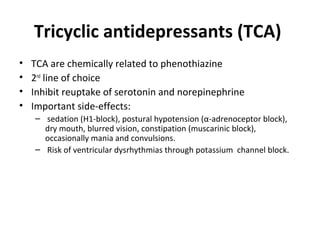
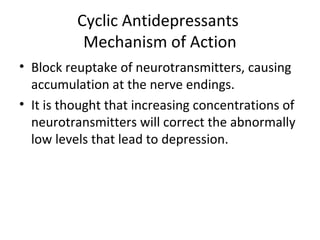
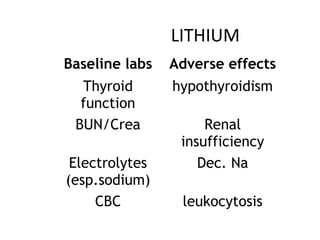
This document discusses drugs used to treat affective disorders such as depression and mania. It describes the mechanisms and side effects of tricyclic antidepressants (TCA), selective serotonin reuptake inhibitors (SSRIs), monoamine oxidase inhibitors (MAOIs), and lithium. TCAs have anticholinergic side effects. Chlomipramine is used for obsessive compulsive disorder. Imipramine causes sedation. MAOIs carry risk of hypertensive crisis. Seizure is a side effect of bupropion.