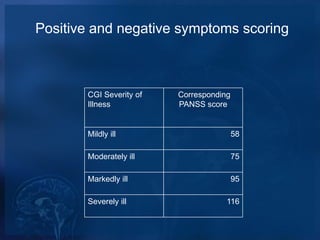
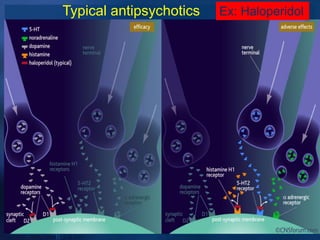
This document discusses psychotic disorders and schizophrenia. It defines schizophrenia as a serious mental illness characterized by illogical thoughts, bizarre behavior, and experiences like hallucinations. The diagnostic criteria for schizophrenia include symptoms like delusions and hallucinations. Positive and negative symptoms are assessed using scales. Treatment involves antipsychotic medications, including typical antipsychotics which block dopamine receptors, and atypical antipsychotics which are less likely to cause motor side effects but can increase risks like weight gain. Clozapine is reserved for treatment-resistant cases due to potential side effects. Patient counseling involves ensuring adherence to treatment and monitoring for side effects or relapse.