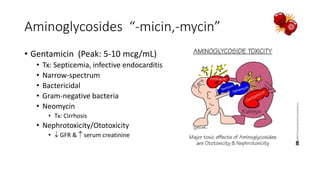
This document summarizes various classes of antibiotics including their mechanisms of action, examples of drugs within each class, common uses, and important considerations. It covers beta-lactam antibiotics like penicillins and cephalosporins which inhibit bacterial cell wall synthesis, as well as other drug classes that target bacterial nucleic acid, protein and folic acid synthesis. Each drug class is described in 1-2 paragraphs outlining representative drugs, spectrum of activity, dosing and key side effects or drug interactions.