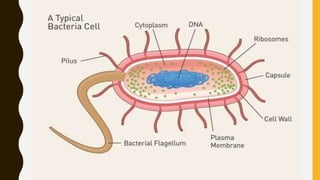
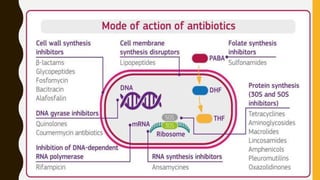
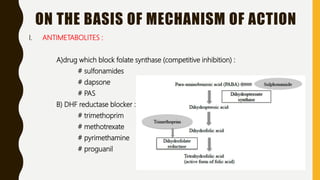
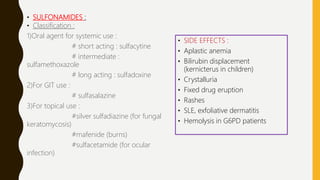
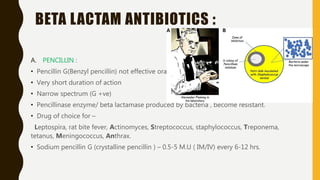
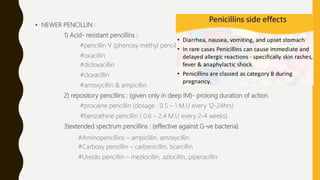
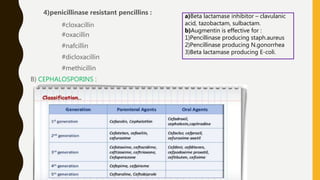
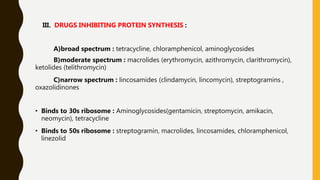
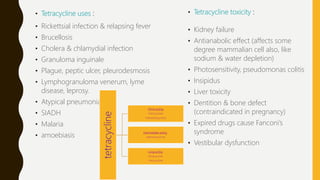
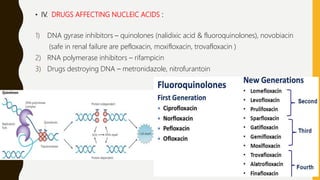
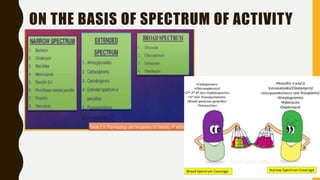
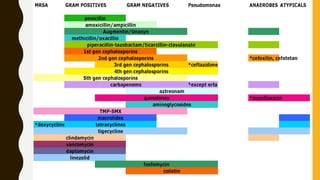
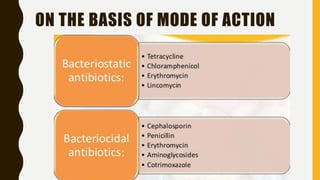
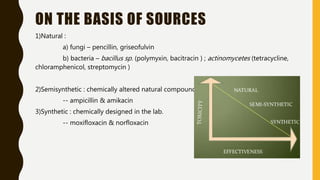
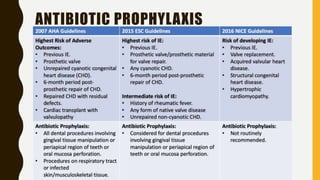
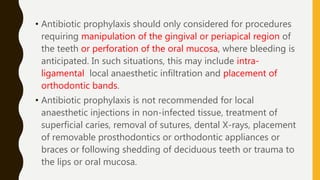
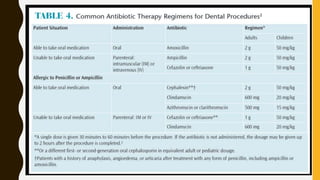
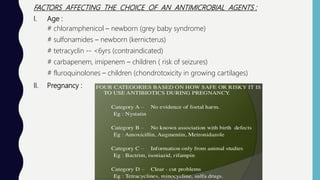
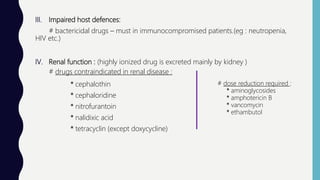
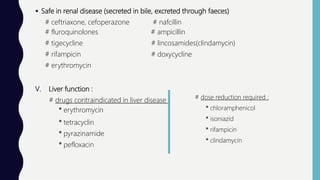
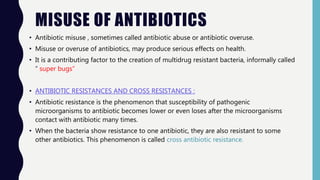
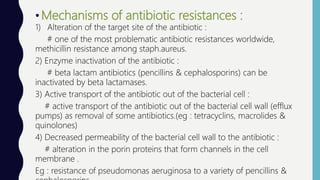
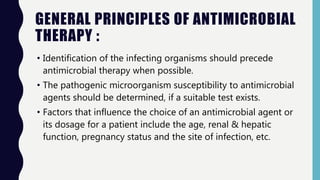
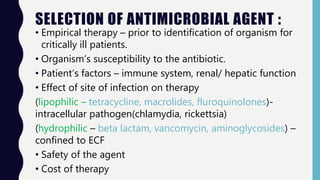
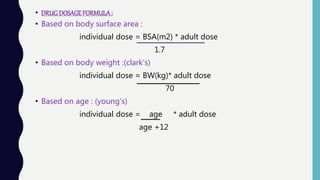
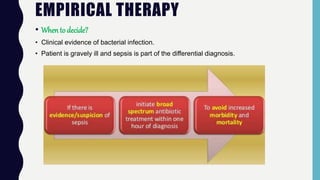
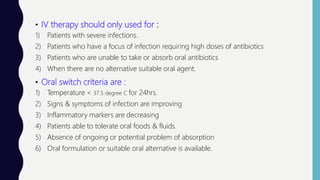
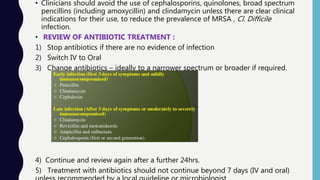
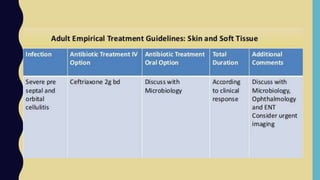
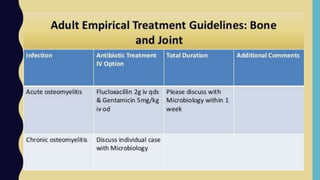
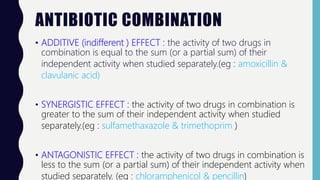
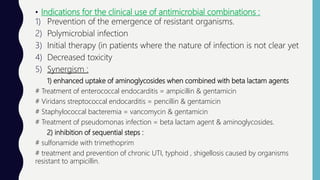
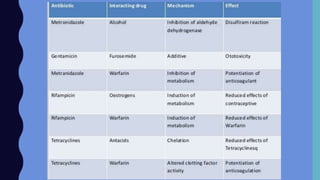
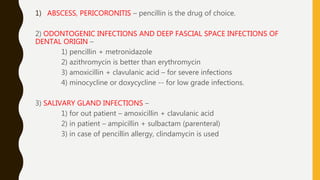
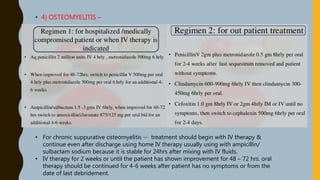
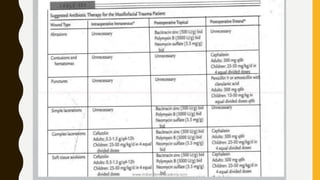
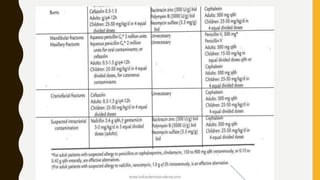
The document discusses antibiotics, their classifications, mechanisms of action, and therapeutic uses in oral and maxillofacial surgery. It highlights the importance of appropriate antibiotic use to prevent resistance and emphasizes factors affecting the choice of antimicrobial agents. Additionally, it covers antibiotic prophylaxis, misuse, and the need for judicious antibiotic therapy to maintain effectiveness.