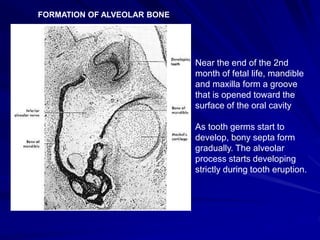
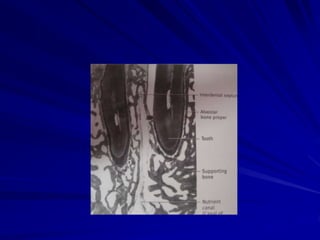
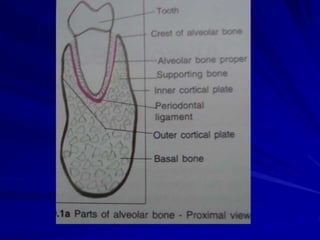
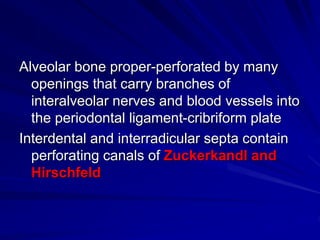
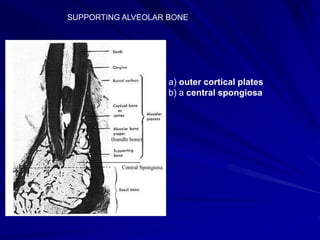
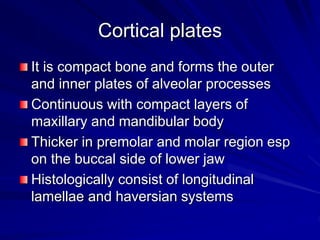
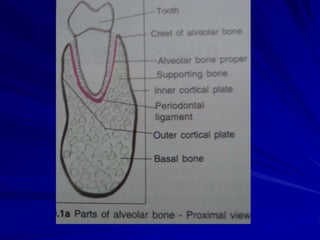
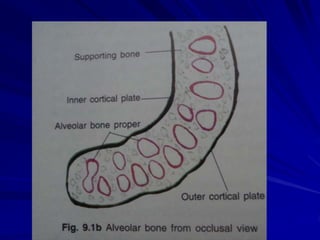
The alveolar process forms the sockets that house the roots of teeth. It has two parts - the alveolar bone proper which surrounds the roots, and the supporting alveolar bone which provides structure. The alveolar bone is remodeled throughout life as teeth erupt and resorb in response to forces. Periodontal disease can cause harmful resorption of the alveolar bone. After tooth loss, the residual alveolar ridge undergoes predictable resorption patterns over time.