The document summarizes key information about alveolar bone:
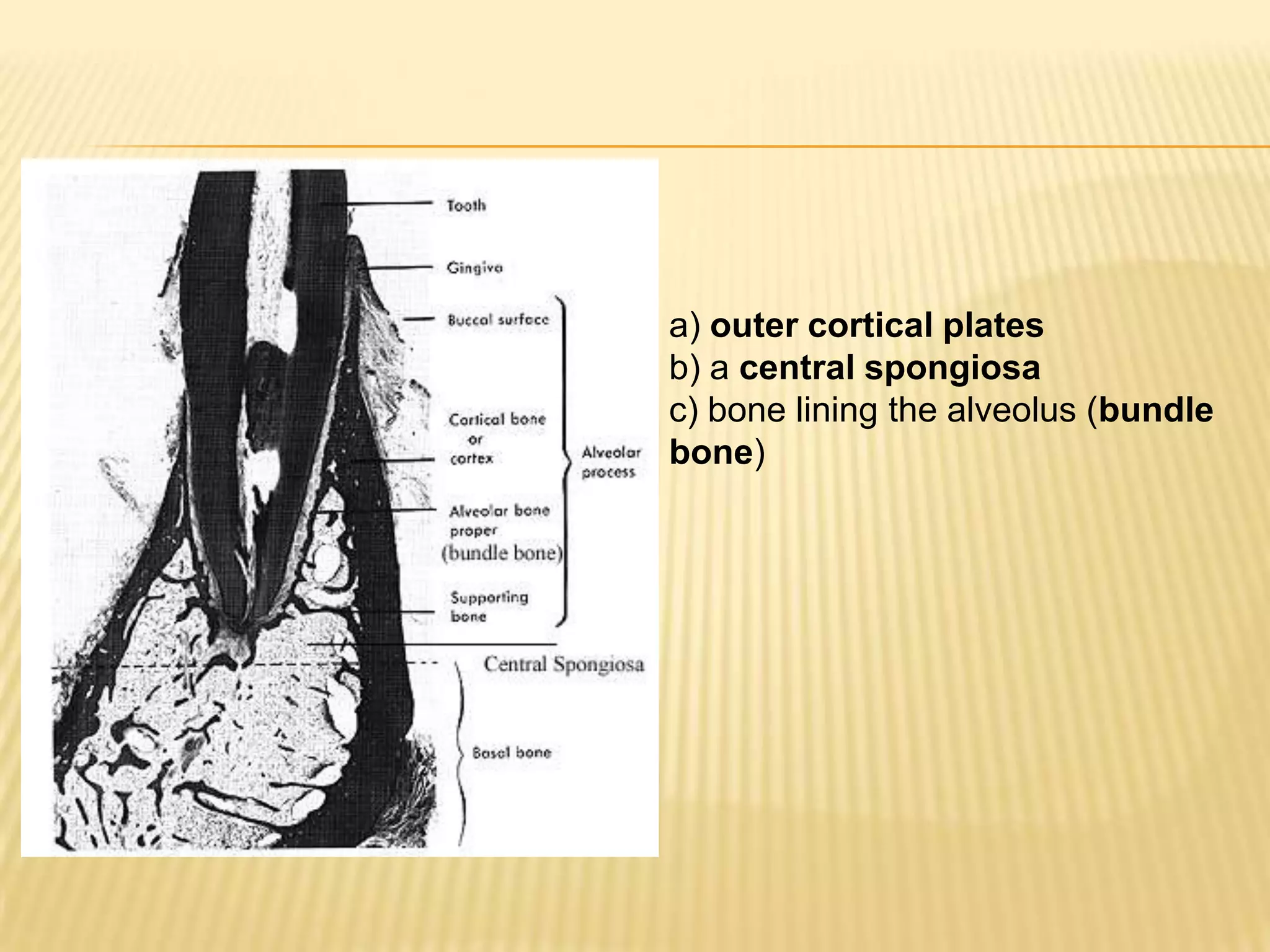
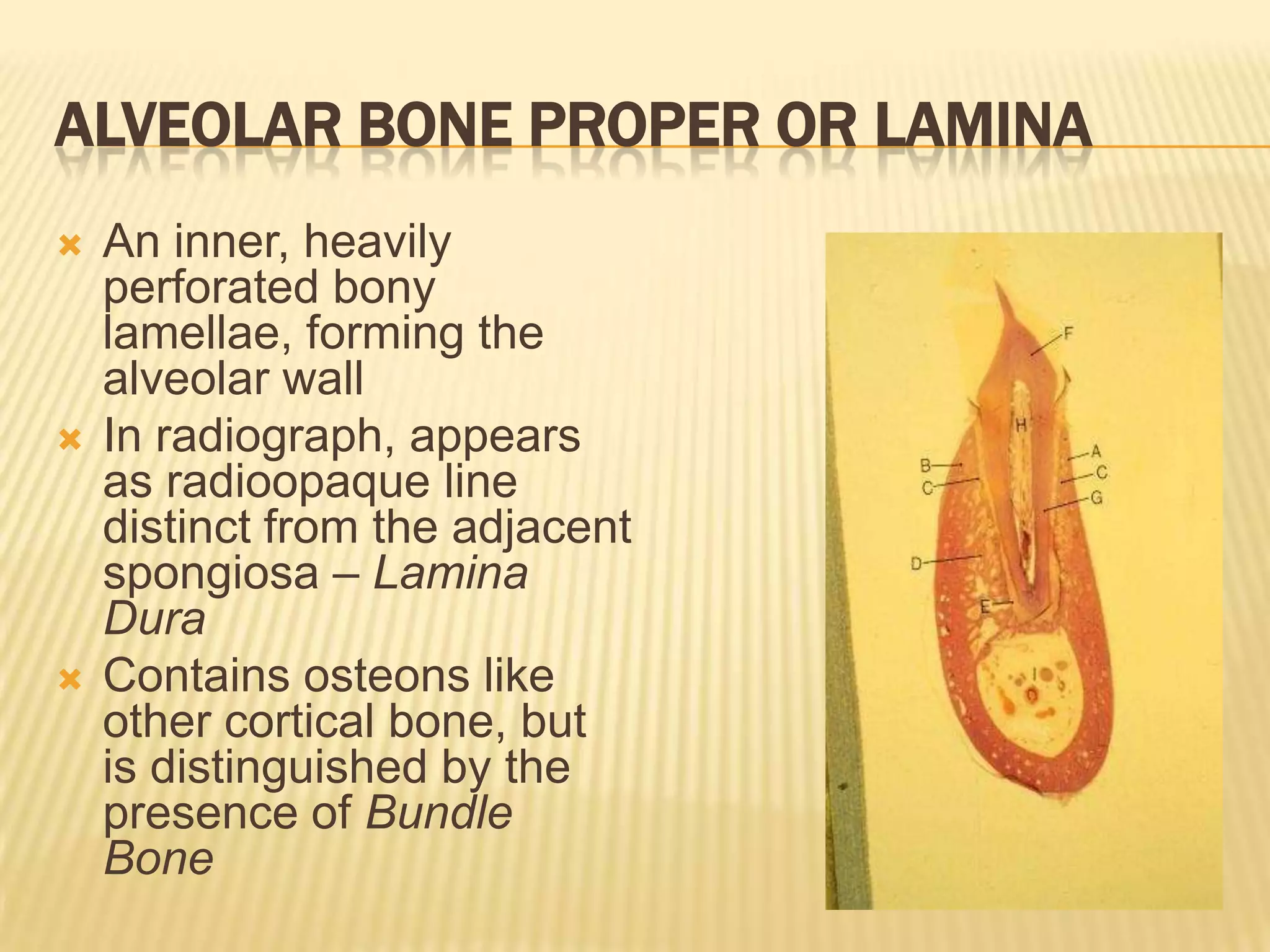
1) Alveolar bone develops from the dental follicle and forms the sockets that hold teeth. It is composed of cortical plates and spongy bone between the plates.
2) The alveolar bone provides protection, attachment, and support for teeth. It also helps absorb forces placed on teeth.
3) Key structures of alveolar bone include the lamina dura lining sockets, interdental septa separating sockets, and Sharpey's fibers that attach the bone to ligaments. Periodontal disease can affect the bone and other supporting tissues.