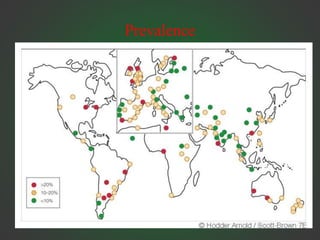
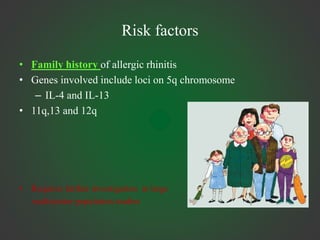
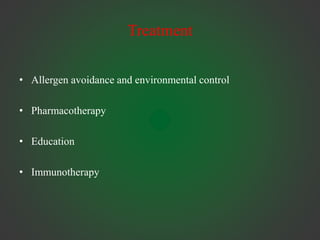
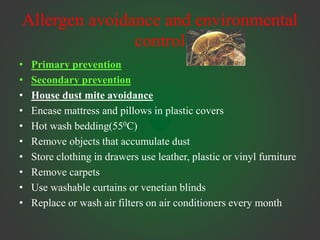
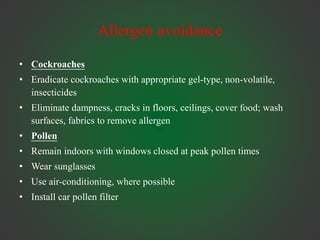
Allergic rhinitis is an IgE-mediated inflammation of the nasal mucosa following exposure to an allergen. It affects 10-30% of people globally. Symptoms include sneezing, rhinorrhea, nasal obstruction, and itching. Diagnosis involves demonstrating IgE sensitivity, usually via skin prick testing or allergen-specific IgE blood tests. Treatment includes allergen avoidance, pharmacotherapy like antihistamines and intranasal corticosteroids, and immunotherapy for persistent cases. Immunotherapy aims to induce tolerance through repeated administration of allergen extracts.







![Immunotherapy
• Efficacy
• In selected patients immunotherapy may be highly
effective[Grade A]
• Upto 50% reduction in symptoms and 80% reduction in rescue
medication
• Treatment for 3-4 yrs results in sustained improvement for at
least 3 yrs following discontinuation[Grade A]
• In a study of children with seasonal rhinitis, immunotherapy
for 3 yrs resulted in a 2-3 fold reduction in the risk of
developing bronchial asthma[Grade B]](https://image.slidesharecdn.com/allergicrhinitis-220922171019-b30628c7/85/allergic-rhinitis-pptx-56-320.jpg)
![Surgery
• Marked septal deviation[Grade D]
• Bony turbinate enlargement[GradeD]
• Mucosal hypertrophy[Grade C]
• Endoscopic sinus surgery [Grade B]](https://image.slidesharecdn.com/allergicrhinitis-220922171019-b30628c7/85/allergic-rhinitis-pptx-62-320.jpg)