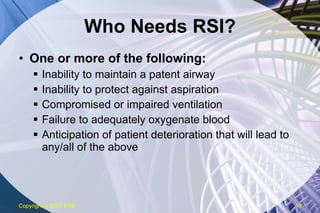
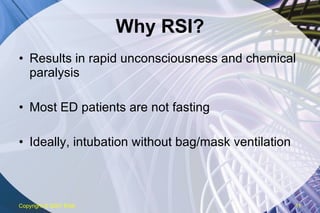
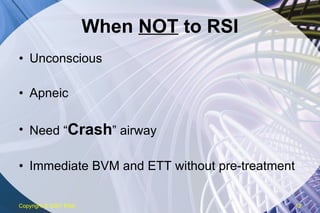
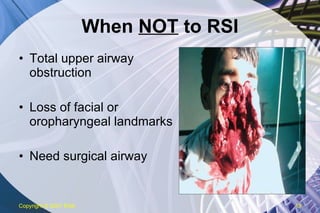
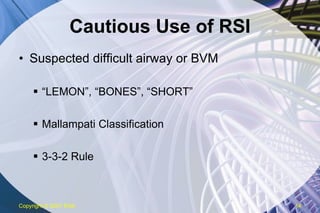
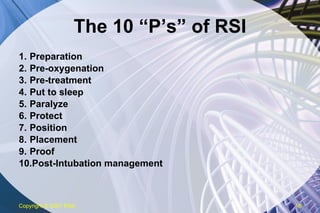
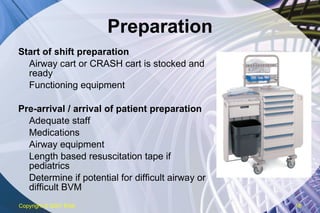
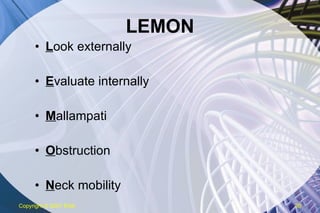
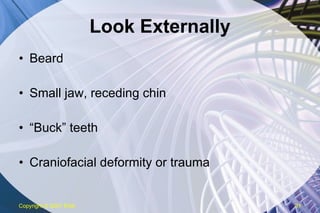
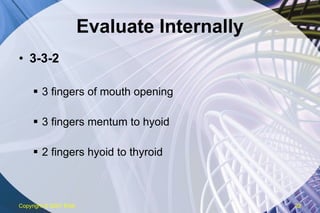
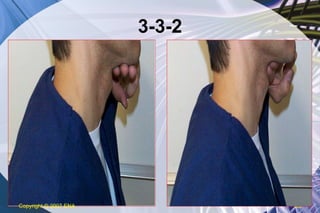
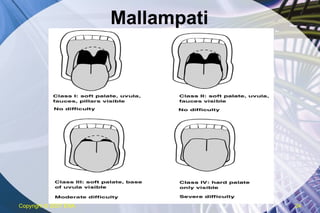
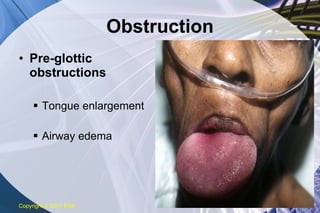
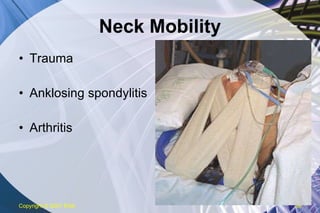
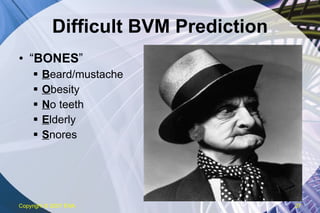
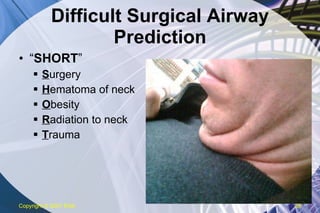
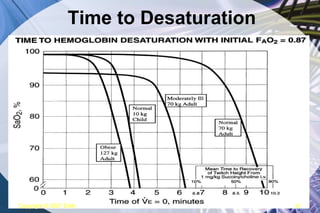
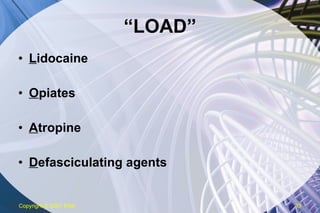
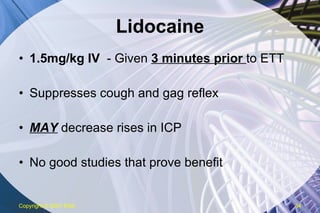
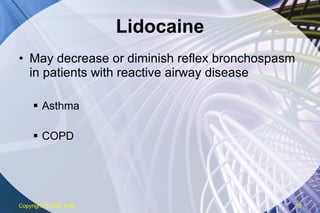
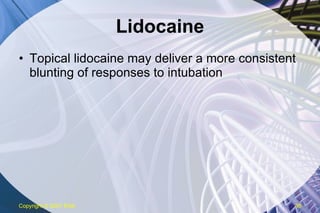
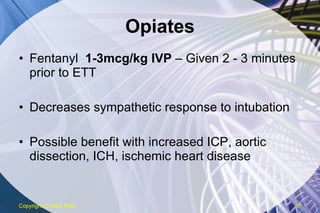
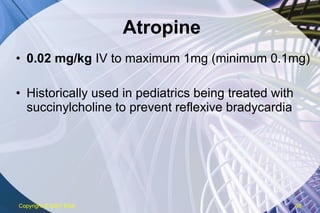
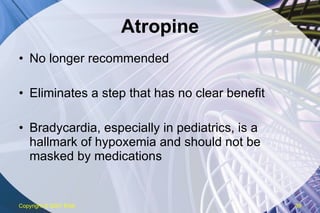
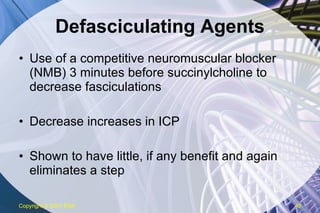
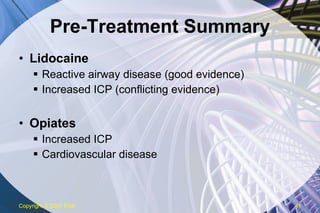
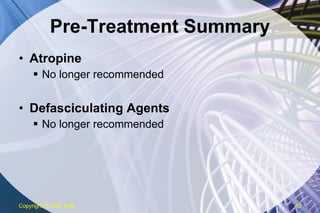
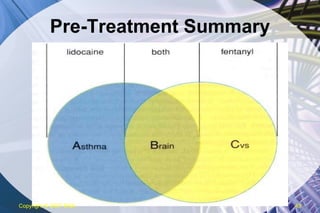
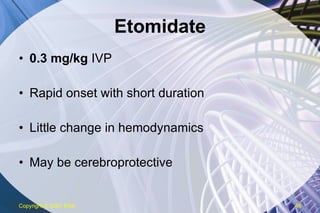
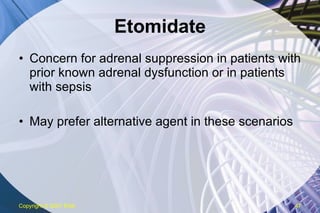
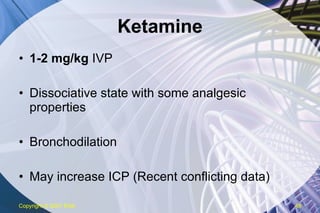
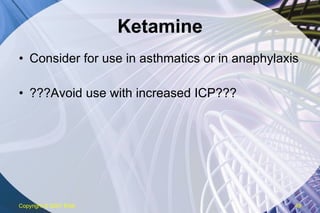
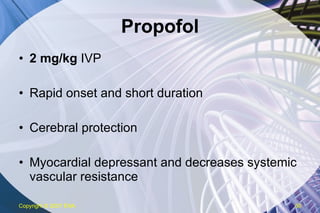
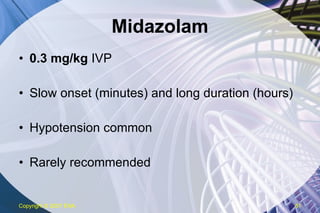
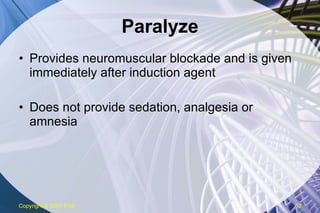
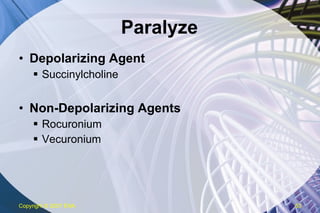
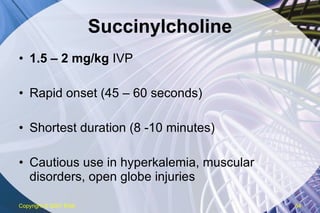
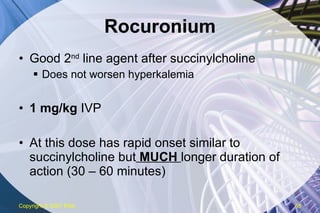
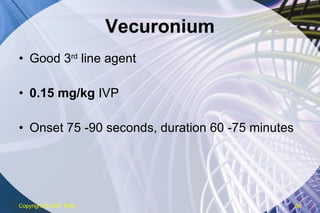
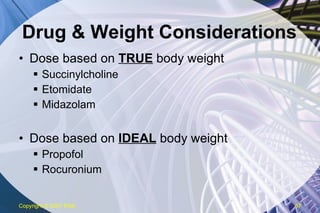
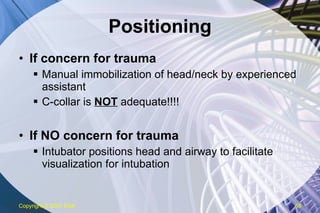
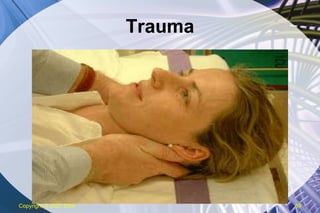
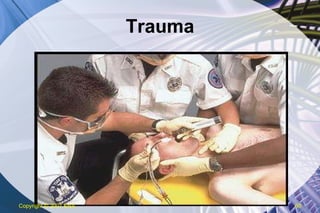
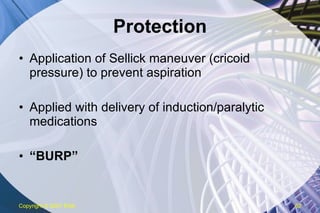
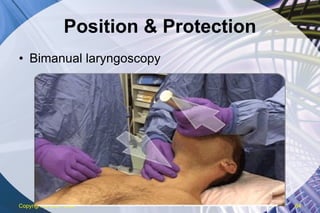
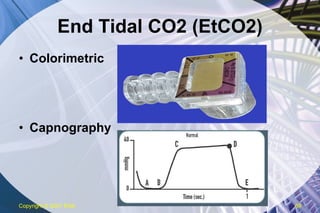
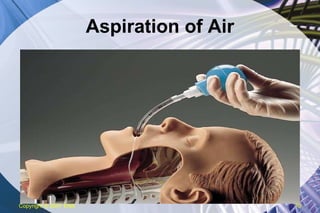
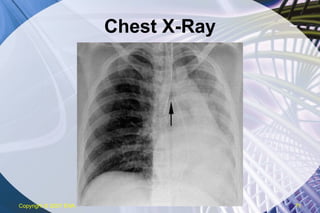
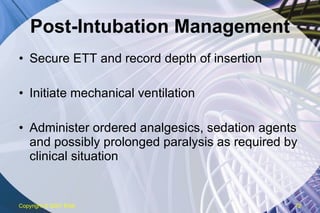
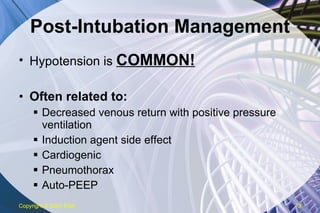
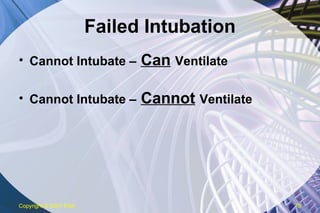
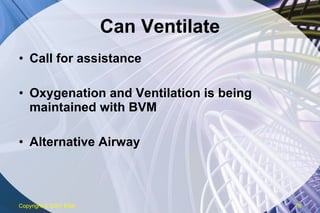
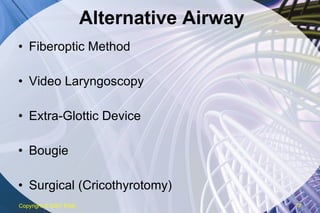
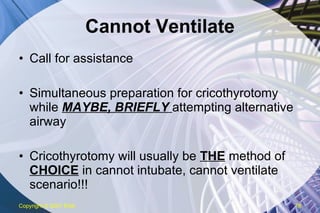
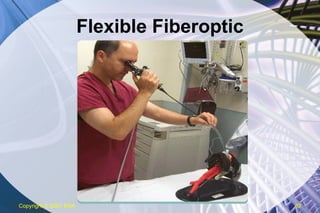
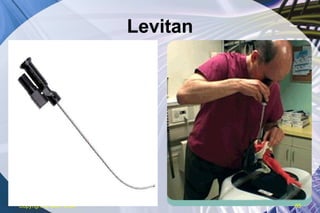
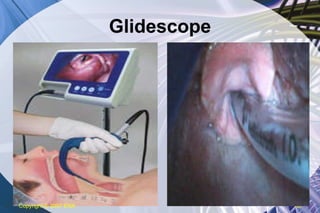
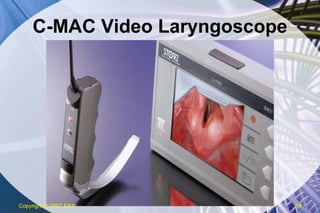
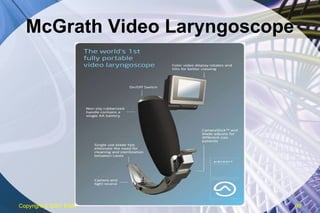
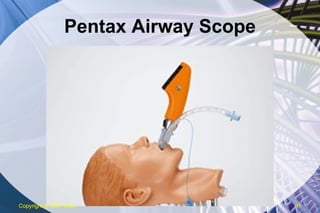
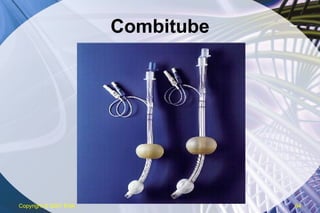
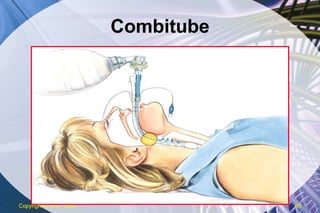
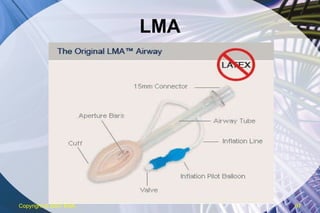
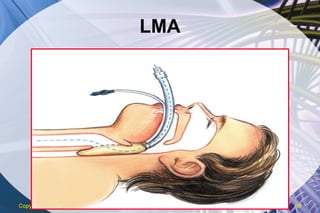
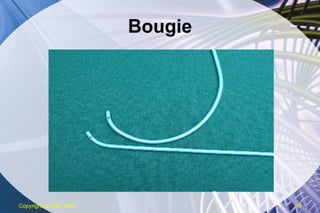
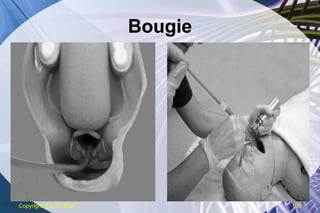
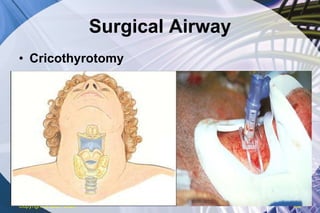
The document discusses rapid sequence intubation (RSI) and failed intubation. It covers the 10 "P's" of RSI including preparation, pre-oxygenation, pre-treatment, induction, paralysis, protection, positioning, placement, proof, and post-intubation management. It also discusses predicting and managing difficult airways and failed intubations, describing alternative intubation techniques like video laryngoscopy, extraglottic airways, and surgical cricothyrotomy. The importance of adequate preparation, pre-oxygenation, and anticipating difficulties is emphasized.