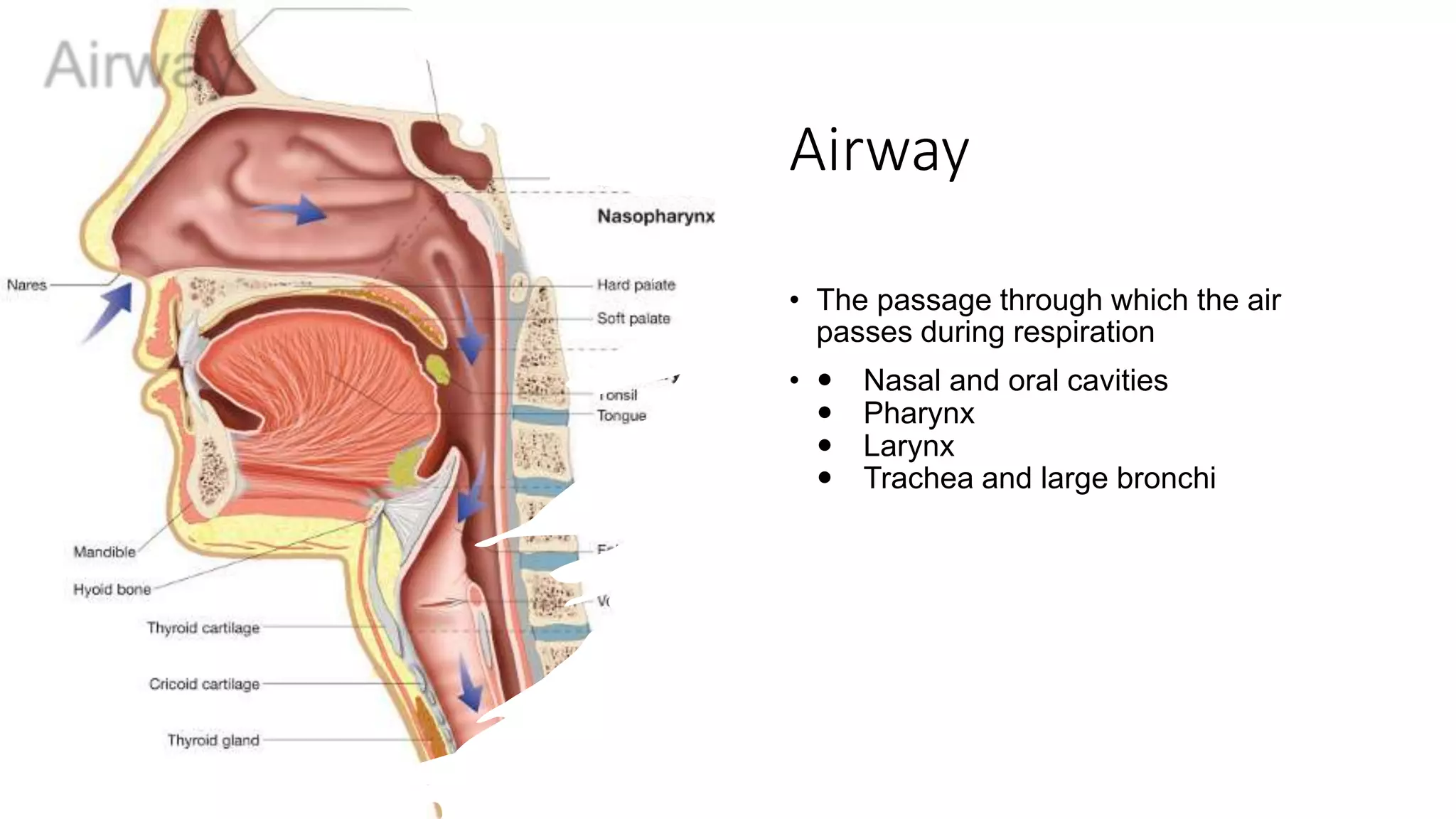
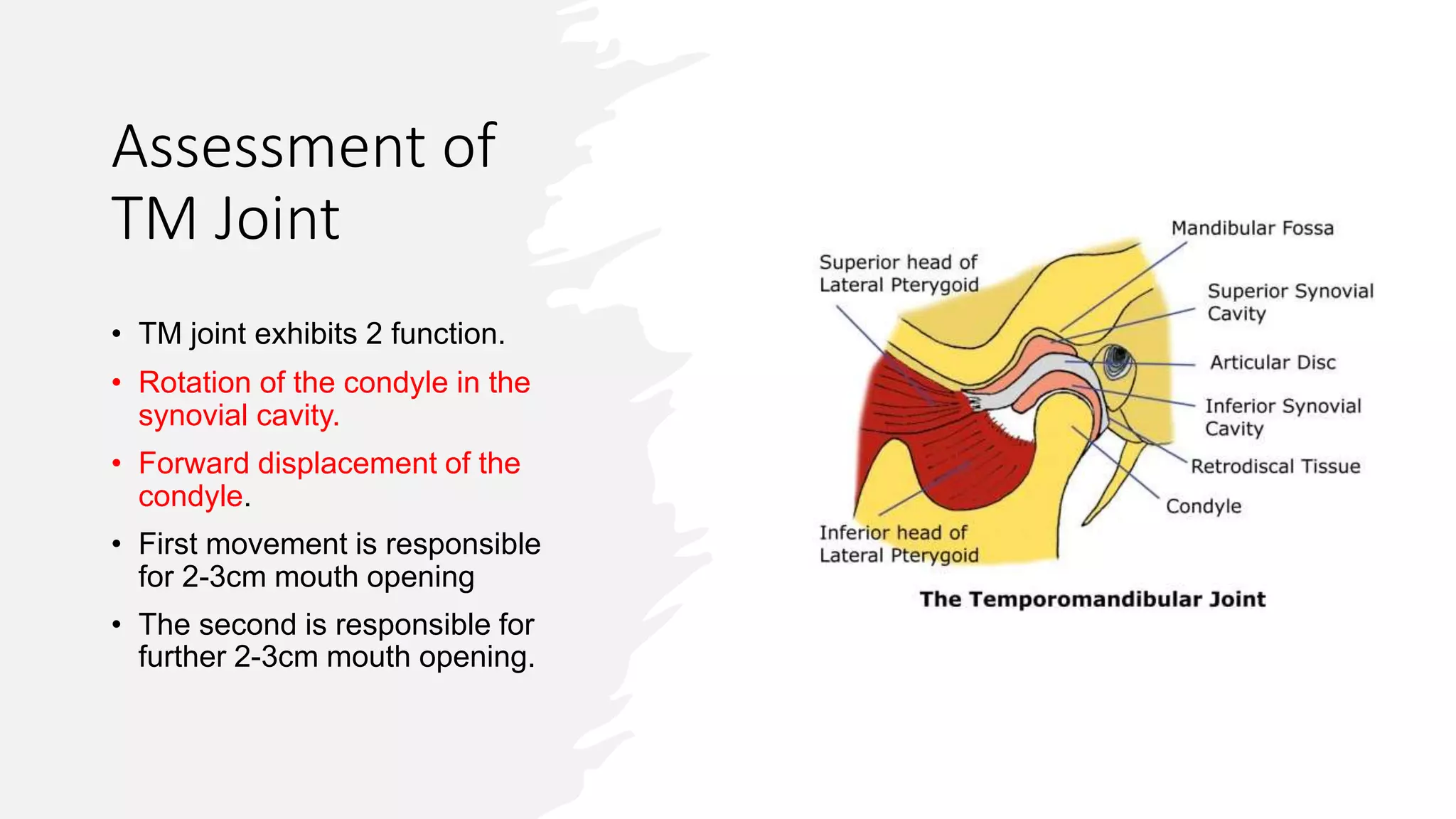
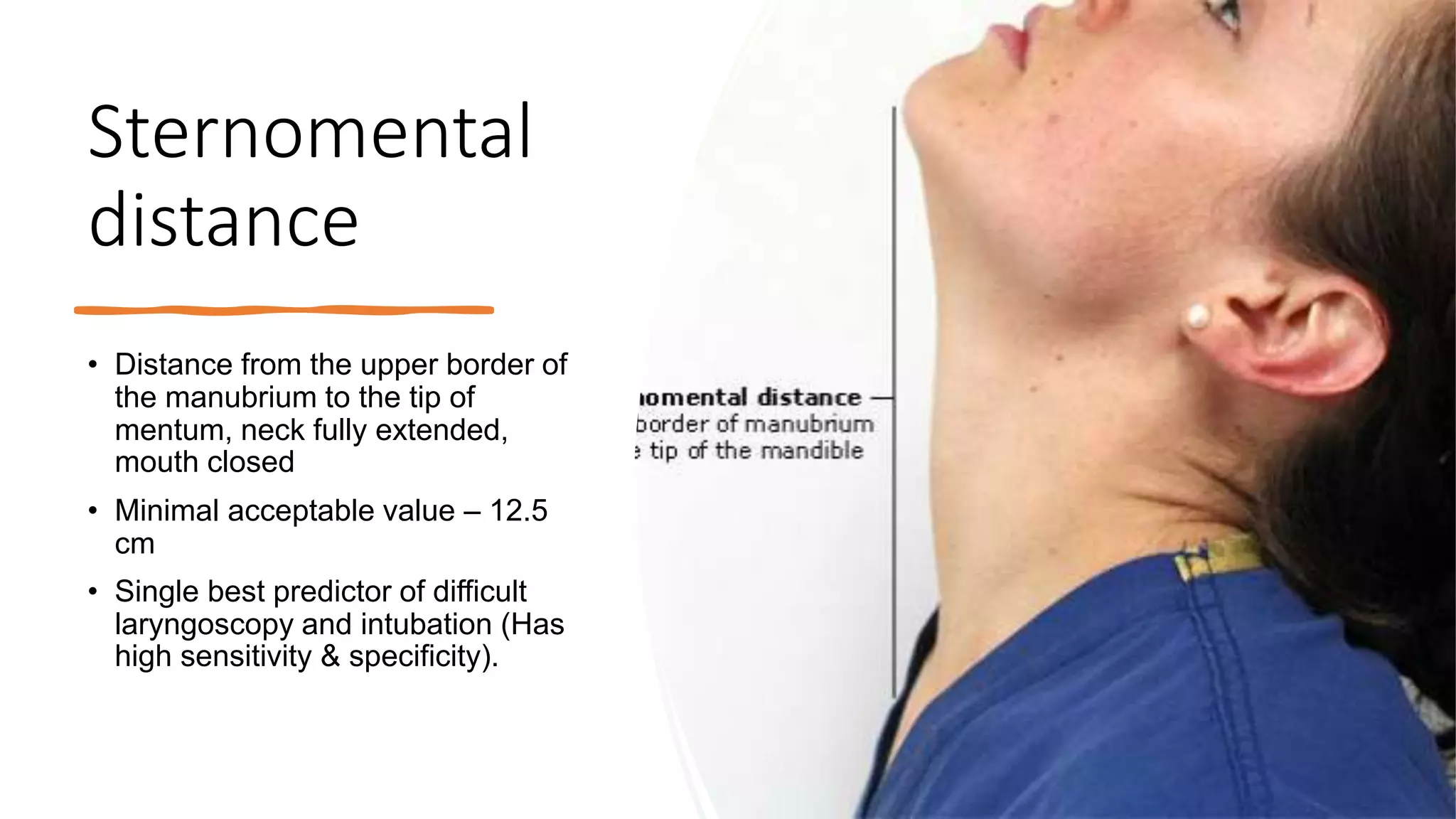
This document discusses the importance of airway assessment prior to anesthesia. It defines a difficult airway as one where a trained anesthetist experiences difficulty with mask ventilation, tracheal intubation, or both. Components of airway examination are described, such as mouth opening, neck mobility, and Mallampati score. Predictors of difficult mask ventilation and intubation are provided. Specific tests are outlined to assess the oropharynx, hyomental distance, thyromental distance, and range of neck motion. Causes and prevalence of difficult airways are reviewed. The document emphasizes performing a thorough airway assessment to predict and prepare for potential difficulties.