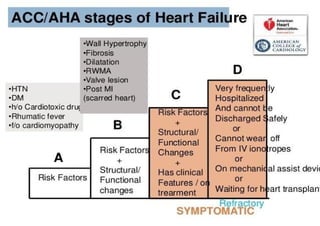
Heart failure is a clinical syndrome characterized by symptoms such as breathlessness and fatigue caused by structural or functional abnormalities of the heart. It is a leading cause of hospitalization in people over 65. Up to 50% of heart failure patients die within 5 years of diagnosis.
The document discusses classifications of heart failure based on ejection fraction and functional capacity. It provides guidelines on the management of acute heart failure, including treatments to reduce congestion and increase perfusion. Chronic heart failure treatment focuses on reducing mortality and hospitalizations through optimized medical therapy including ACE inhibitors, beta-blockers, MRAs, and newer drugs like sacubitril/valsartan. Device therapies like ICDs and CRT are recommended for