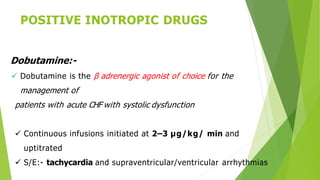
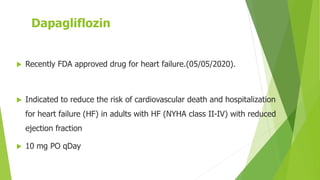
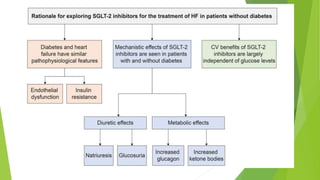
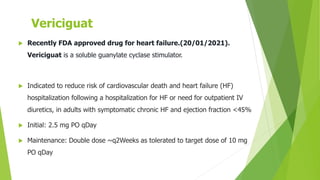
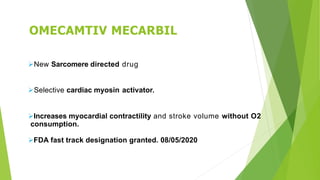
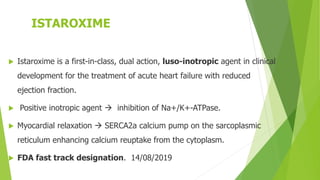
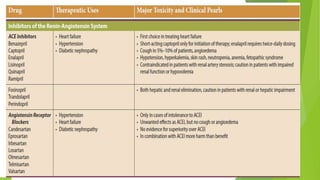
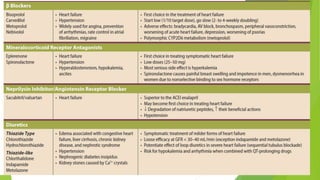
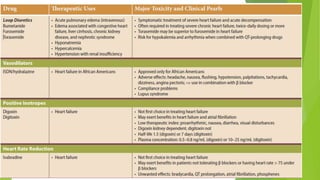
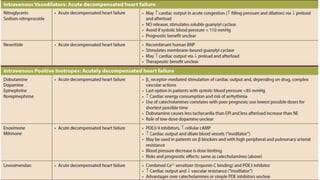
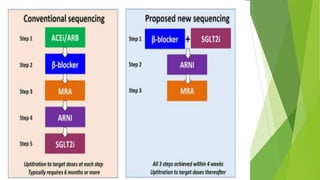
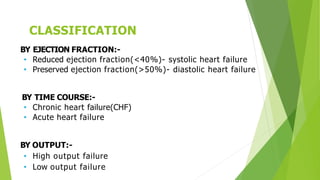
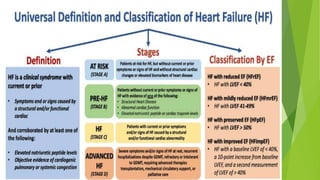
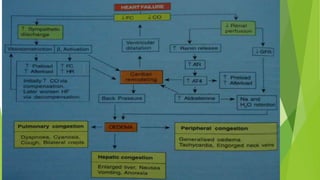
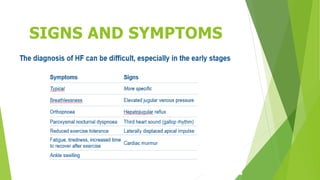
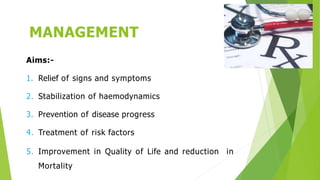
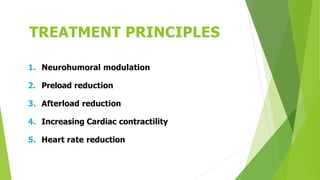
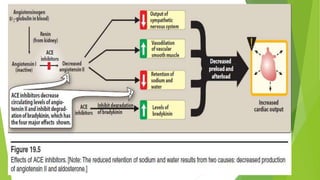
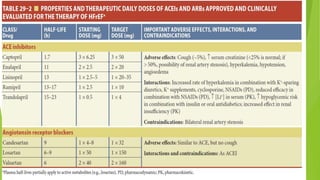
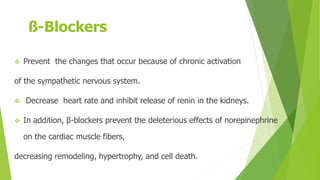
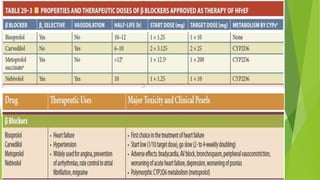
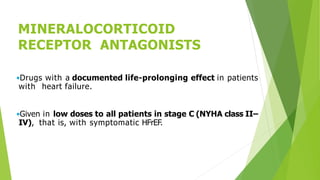
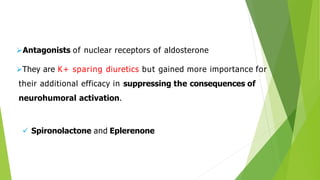
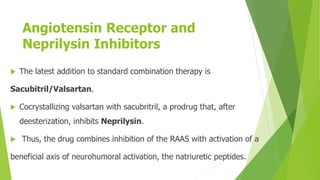
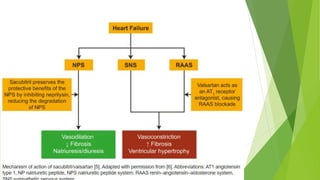
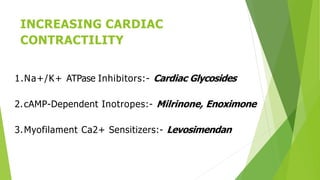
The document summarizes recent trends in the management of heart failure. It discusses the epidemiology and classification of heart failure. The mainstay of treatment involves neurohumoral modulation using ACE inhibitors, ARBs, beta-blockers, and MRAs. Other management principles include preload and afterload reduction, increasing contractility cautiously, and reducing heart rate. Newer drugs like sacubitril/valsartan, dapagliflozin, and vericiguat are improving outcomes, while others like omecamtiv mecarbil and istaroxime are under investigation.




![Actions of Digoxin:-
Positive Inotropic Effect by raising intracellular [Ca2+] and
enhanced contractility
This Increased cardiac output provides symptomatic relief in
patients
with heart failure](https://image.slidesharecdn.com/recenttrendsinheartfailure-220708062757-e0353f6b/85/recent-trends-in-heart-failure-pptx-33-320.jpg)