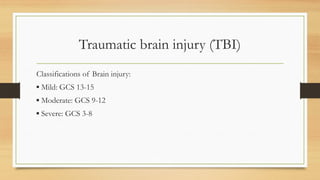
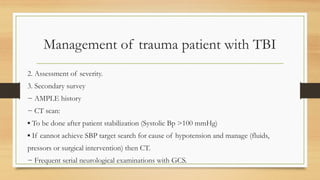
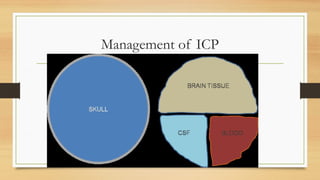
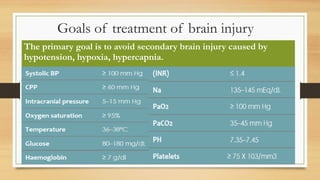
The document outlines the Advanced Trauma Life Support (ATLS) management protocols for trauma patients, emphasizing a systematic approach through primary, secondary, and tertiary surveys to assess and address life-threatening conditions. Key components include airway management, breathing, circulation, and disability assessments, along with specific techniques for different injuries and patient populations, such as pregnant women. It also discusses the management of traumatic brain injuries and complications associated with trauma care.