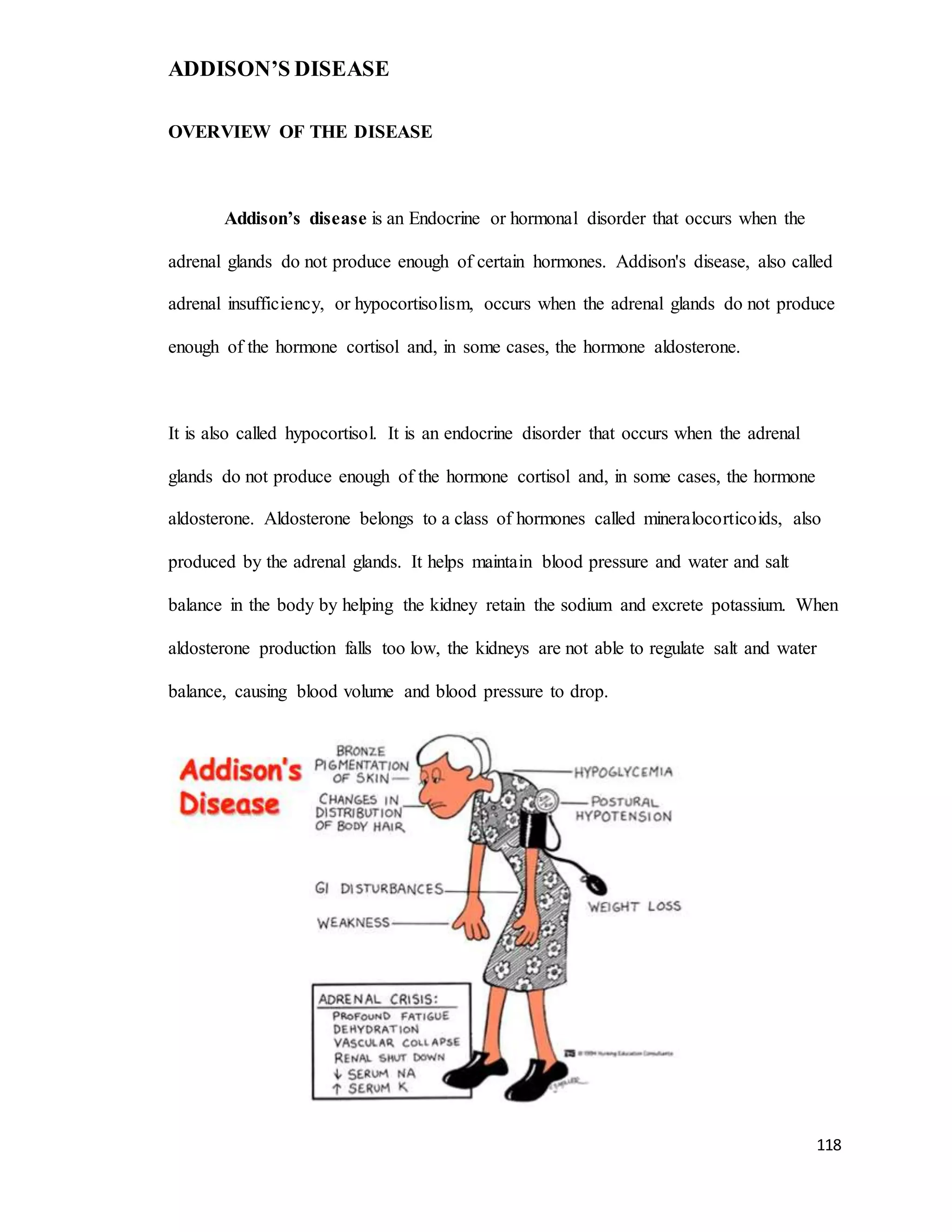
Addison's disease is an endocrine disorder caused by insufficient production of cortisol and sometimes aldosterone by the adrenal glands. It results in symptoms like weakness, fatigue, weight loss, low blood pressure, and hyperpigmentation. Most cases are due to autoimmune destruction of the adrenal cortex. Treatment involves replacing cortisol and aldosterone through medications like hydrocortisone and fludrocortisone. Patients must be monitored for adrenal crises and taught to avoid stress and take medications as prescribed for life.